Sit up straight! Improving work ergonomics to decrease pain, increase energy & productivity23/3/2022 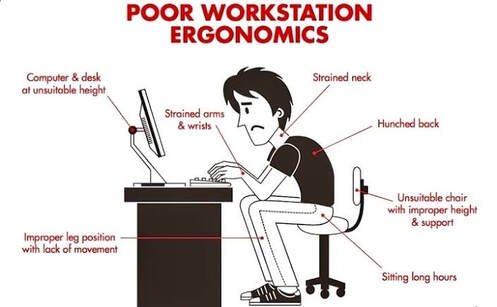 By Angus Nicol Slouchy slouch - How are you sitting? Ever heard of the saying “sitting is the new smoking?” As the health conscious reader I know you are (since you’re reading this blog), I’m almost sure you have. And it’s true, prolonged periods of “sedentary” behaviour (physical inactivity) over long periods can have detrimental effects on both your physical and mental health. This is worrying, since an estimated 81% of Australians work in occupations that require some sitting, with over half of Australians reporting that they sit for work “all the time” or “often”. Today I’m not here to lecture you about all the health consequences of sitting (that may have to wait for another time), but rather to give you some hints and tips about proper desk posture and ergonomics - so that when you are sitting, at least you’re doing it in the healthiest possible way! I feel this is becoming increasingly important given that there are more people than ever working from home in less than ideal workspaces (whether that be in bed/on the couch, at the kitchen table etc). I’m sure you would all recognise the classic “desk posture”. Generally what you will see is four basic characteristics in the upper body:
This happens because when we’re sitting at a desk, everything we need is in front of us, so we slouch to get closer to it. This causes the muscles in the front of our chest to become short and tight and holds us in this rounded shoulder position. The opposite happens to the muscles in our back, over a long period of time the muscles between our spine and our shoulderblades may get weak and lazy, and they may no longer have the strength or endurance to hold our shoulders backwards. This contributes to the upper part of the back becoming increasingly rounded and stiff, making it hard to sit up tall. This means that to continue looking straight ahead, you have to tilt your head backwards slightly. This requires excessive use of the muscles in the base of your skull and back of your neck and they may then become tight and give you neck pain. These muscles also refer up towards your skull, so tightness in these muscles may also be responsible for headaches! I feel it’s important to note that stress commonly causes these muscles to become tense, and exacerbate your neck pain and headaches. Have a look in the mirror - look front-on and side-on, and notice the position of your shoulders, the curve in your upper back and the position of your neck. Does any of it fit what I just described? Well fear not, you’re not alone. This is one of, if not, THE most common complaint I see in practice… but the good news? YOU CAN DO SOMETHING ABOUT IT!  Ergonomics 101 - The quick fixes A good place to start is by checking your work/desk setup… because if this isn’t ideal, chances are you’re going to be fighting an uphill battle. Where possible (and I know it may not always be!), try to have a dedicated area that you work from if working from home. Try to avoid sitting on surfaces that are too soft (eg beds or soft couches), as these are sacred bits of furniture that should be used for relaxation and enjoyment purposes only! Not to mention they are a posture nightmare! Here are some tips to try and ensure good posture when sitting at your desk. If possible, read this next part at your desk, and make adjustments as you go. It should only take a couple of minutes, and could save you a lot of pain and discomfort!
 Need some help? Here are some people and gadgets to assist you. Okay, how are you feeling now? Although it may seem relatively straightforward, getting this right can be a bit tricky. Sometimes some problem-solving, a bit of imagination and a helping hand is necessary. So, if you’re still struggling to achieve an ideal desk setup, it might be time to try to enlist some help. There’s a few ways you can go about this! First of all, take a photo of your current desk setup (ideally from side on with you sitting in it) and bring it into your local osteopath! We may be able to offer tailor-made advice and recommendations to perfect your desk setup. Other healthcare practitioners such as physiotherapists, chiropractors, GPs and occupational therapists (OTs) may also be able to offer sound advice! Furthermore, there is an overwhelming amount of gizmos and gadgets out there designed to help improve your work ergonomics and make you as comfortable as possible. There is anything from ergonomically designed seats, sit-to-stand desks, ergonomic mouses and keyboards, footstools, back braces and much more! However, not all of these may be necessary for you, and there are some dodgy ones out there, so I highly recommend consulting your local healthcare practitioner to assess what may be useful for you, before wasting money on expensive fancy and potentially unnecessary things! Another little hot tip… many large corporations (and even some small-medium organisations) employ professionals to perform ergonomic assessments, so it may be well worth your while and a good excuse to stand up and go for a wander to HR, or to your managers office, and ask if they can get someone to inspect for you. Sometimes workplaces are willing to cover expenses for any equipment that you require too! Because after all, happy, pain-free employees are likely to be more productive and make them more money… so your comfort is in their best interests too!  Visit your osteo! Great! So now you have a perfect desk setup. But wait… there’s more. Think about your current job, and previous jobs before that. Do you think you could calculate the time spent sitting (probably with poor posture)? Guess what, a new desk setup isn’t magically going to reverse years of poor posture! BUT some hands-on treatment and some simple, easy exercises may help. Osteopaths can assess the main cause of your pain/discomfort and provide manual therapy and personalised exercises to help alleviate your pain, headaches and improve your posture! We may also take into account any other factors that may be influencing your pain (eg stress levels, diet & sleep etc). However, from a purely biomechanical perspective, an osteopaths goals may include:
Most of the time, postural complaints are not something that can be fixed instantly. Things that have been there for a long period of time often take a while to resolve. However, with a little bit of hands-on treatment and some dedication to rehabilitation exercises, you can see significant improvements in pain and headaches within 2-8 weeks… which is not long considering how long it may have been an issue for! Please see below for a few easy exercises you can do whilst at your desk, however this is just the tip of the iceberg, come and see us for a more personalised and comprehensive approach tailored just for you!
0 Comments
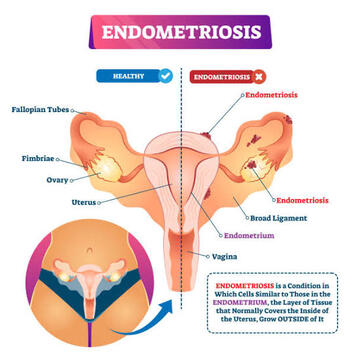
By Liam Neyland As march is Endometriosis awareness month, we at HMC Osteopath’s thought it would be a great time to share some helpful information about this condition. What is Endometriosis? A fair few of you may be wondering what exactly is Endometriosis? Despite the condition affecting approximately 1 in 9 women before they hit their 40’s in Australia, it is a relatively unknown condition within the public. Simply put endometriosis is when cells (endometrium) that usually line the cavity of the uterus, better known as the womb, grow in other parts of the body. These cells can occur at almost any site within the pelvis, but is most commonly found to be sitting on the peritoneum of the pelvis, behind the vagina and uterus, underneath the ovaries and sometimes on the ovaries themselves. In it’s more severe forms this condition can even grow inside the Fallopian tubes or even within the ovary itself. However, there have been cases where these cells have been found outside the pelvis like for example the lungs (thankfully these cases are extremely rare). Despite the fact these cells are not present in the uterus they still respond to hormonal messages from the ovaries. This is especially true during the menstruation period of a women’s cycle, as these cells will bleed every month resulting in inflammation, scarring and in some cases organs to stick together. It is for this reason why women suffering from endometriosis can have such debilitating pain. Along with debilitating pain the disease can affect fertility. How does Endometriosis affect Fertility? The link between fertility and endometriosis is unfortunately unclear, however the stage of the condition and location do play a major role on possible fertility issues. Examples of this are if extensive scarring within the pelvis could result in pain during intercourse, lowering a women’s enjoyment and or dreading the act of intercourse as a whole. Another example would be the Fallopian tubes could become tangled in the scar tissue limiting it’s ability to safely transfer the egg from the ovary to the womb. These are two of many possible outcomes that endometriosis can effect a women’s fertility. Thankfully, many women with this condition can still become pregnant as an estimated 70% of women with mild to moderate endometriosis get pregnant without the use of external treatment. 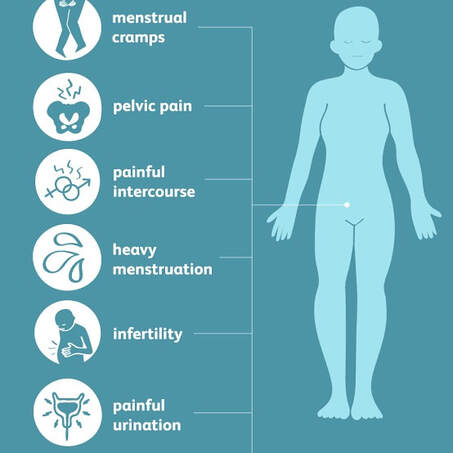 What are the Symptoms of Endometriosis? The symptoms that women experience while suffering from endometriosis will be different by a case to case matter. As the severity of the condition does not necessarily coincide with the symptoms felt but instead where the lesions are located. Common Symptoms include:
What causes Endometriosis? Currently there is no known cause of endometriosis, however factors that increase the likelihood of the condition are as follows.
 How is it Diagnosed? Unfortunately due to difficult it is to identify many women go undiagnosed for many years with the average being around 7. Currently the only way to confirm a diagnosis of endometriosis is to have a laparoscopy, which is a particular surgery where doctors are able to look for endometriosis tissue within the abdomen and take a sample to examine in a laboratory. During the surgery the grading of endometriosis would be determined as well. Grade 1 (mild): small patches scattered around the pelvis Grade 2/3 (moderate): disease is more widespread and can be found on ovaries and other parts of the pelvis. Grade 4 (severe): Has spread to most of the pelvic organs. If you suspect that yourself or someone else may have endometriosis, please talk to your doctor about any and all symptoms you may be experiencing. A helpful tool has been designed to help health professionals and yourself in identifying and assessing endometriosis symptoms, which may also reach a faster diagnosis. It is called the Raising Awareness Tool for Endometriosis (RATE), which can be accessed through the provided link. RANZCOG - RATE What are your treatment options? Conventional treatment of endometriosis is wide ranging as not all therapies may be effective or the possible side effects could have an overall net negative for a person’s health. It is important to discuss with your doctor about any and all side effects with any treatment options. As stated in the previous blog, currently there is no cure for endometriosis, so in that regard all treatments are aimed at pain management or general management of the condition. Non-manual therapy treatment option
Hormone Therapies, are used to help suppress the growth of the endometrial cells and stop or limit bleeding, including during the menstrual cycle. Examples include:
Surgery: aim is to remove as much visible endometriosis as possible and to repair any damage found.
 Self care treatment It is important to remember that the pain and or discomfort a women may experience from Endometriosis is unique to them and will vary from person to person. With that in mind here are some examples of at home treatments you can use to help with managing your pain. Exercise
Other supportive self care treatments are:
What can my Osteopath do? When treating endometriosis, it is best that a multi-disciplinary approach is used. Where a range of health professionals including your GP work together to provide the best possible care for you. Osteopathy would provide a range of hands on, non-invasive treatment methods to best optimise the body’s natural function. Examples of possible treatments that an Osteopath could provide you are as follows.
 What can my friends and family do to help? The best thing that friends or family can do to help is be a reliable source of support. Many people suffering from endometriosis feel alone in their struggles. Something as simple as bringing your loved one a heat pack when you notice them struggling or allowing them to sleep in a little longer can go a long way in helping someone suffering to feel more validated. Always remember that just because you cannot see the illness does not mean that it does not exist. It is important to remember that symptoms for endometriosis are varied and unique to the individual and that the condition does not have a set rhyme or rhythm. So please be understanding that someone with this condition cannot control or predict when a ‘flare’ will occur. References
How does endometriosis affect fertility? | Tommy's (tommys.org) Where Does Endometriosis Occur | Gynaecology Molloy Endometriosis | healthdirect Endometriosis (who.int) Exploring effect of pain education on chronic pain patients’ expectation of recovery and pain intensity (degruyter.com) Management & treatment of endometriosis | Jean Hailes Treating endometriosis | The Royal Women's Hospital (thewomens.org.au) Endometriosis Australia | Home |
HMC TEAMIf you find something of interest that might suit this space, or would like information on a specific topic, let us know at hmcosteo@gmail.com
Archives
December 2023
Categories |

 RSS Feed
RSS Feed
