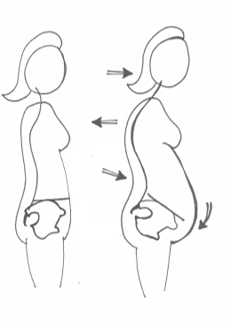
 By Ramona Packham Pregnancy demonstrates the body’s incredible ability to adapt to change, nurture growth and produce life. As a baby grows, the mother’s body changes to create more space. Organs get squashed, the diaphragm moves up, the rib cage widens, the muscles of the back work overtime to compensate for the muscles at the front being stretched, the curves in the spine increase, and the pelvic floor takes on an increasing amount of downwards pressure. Given all these wonderful changes, it is not surprising that some pregnant and post-partum women experience conditions that can cause discomfort, pain, stress, and anxiety. Incontinence, separation of the abdominal muscles, and scarring are three of these conditions, and there are strategies available to assist in recovery. The Pelvic Floor Let’s revise an important structure relevant to these conditions, the pelvic floor. Have you ever been told to strengthen your ‘core’ muscles? A lot of people perceive this as the six-pack muscle between the ribs and pelvis. While this muscle forms part of the core, it is just one piece in the puzzle. Think about your core as a cylinder. The broad diaphragm muscle that allows us to breathe forms the roof, and the pelvic floor forms the floor, hence its name! The pelvic floor supports the bladder, uterus, and bowel, and facilitates the birthing process. As a baby grows, the downwards pressure on the pelvic floor increases. The pelvic floor also works to maintain continence, and functions hand in hand with the abdominal muscles. In the pregnancy and post-partum population, the pelvic floor creates a passageway for the baby to move through in birth and helps to maintain continence afterwards. Incontinence Approximately 33% of women experience bladder or bowel incontinence after giving birth. While this is an outcome for some pregnant women, it is not inevitable, and it is recoverable. If you suffer from incontinence, seek help. The health of the pelvic floor affects both bladder and bowel continence. The pelvic floor can be weak and underactive or tight and overactive and both can lead to incontinence and produce similar symptoms. If you have a weakened or underactive pelvic floor, symptoms include the feeling that you just can’t hold on when needing to go to the toilet, or accidentally losing control over your bladder or bowel. On the other hand, if your pelvic floor is tight or overactive, you might experience painful sexual intercourse, pelvic pain, straining when going to the toilet, constipation or a feeling of incomplete emptying, or stress incontinence when participating in certain types of exercise, coughing, sneezing, or laughing, It is important to find out the type of incontinence and the reason for it as this will be a guide to the most effective management. Many women recover from incontinence following pregnancy without doing anything specific, as the tone of the pelvic floor often improves by itself over time. However, there can be residual weakness and recovery can be enhanced with the implementation of simple, time-effective techniques, including pelvic floor and postural work. Postural changes can reduce leaking in women with stress incontinence. Some postural elements a health professional will assess include:
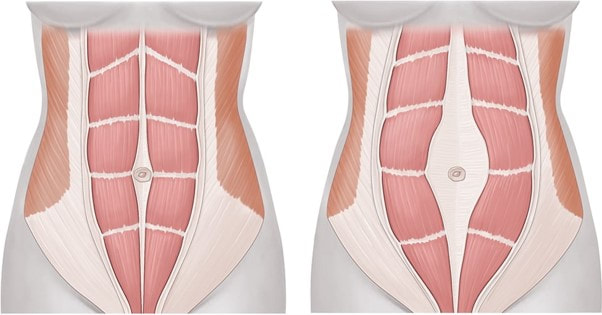 Diastasis Recti A diastais recti (DR) is a separation of the large ‘six-pack’ muscle in the abdomen where it joins in the middle of the trunk at a line called the linea alba, a sheet of connective tissue between the muscles. A DR can also be linked to weak pelvic floor muscles. Some separation is normal in pregnancy, and it occurs as the uterus grows and the abdominal muscles stretch. 100% of women have some diastasis at their due date, but most resolve within 6 weeks post-partum. 39% will still have some diastasis 6 months post-partum, and these women are more likely to have urinary incontinence. A DR does not need to be a lifelong condition, they can resolve with time and management. The linea alba requires some training to repair, just like muscles need to be strengthened after injury. The aim is to activate the deep abdominal muscles and pelvic floor, and then to improve the relationship between these groups. This can be achieved through practicing specific exercises. When completing any exercise with a DR, it is important to monitor for bulging in the space of the DR as this indicates that the muscles may not be contracting as well as they could be. Practice: Observe how flat your abdominal muscles are. Tense your abdominals using your hands to feel what is happening. When you contract, your abdominals should stay nice and flat, and there should not be any bulging outwards. It is likely that during pregnancy you will need to reduce the amount of exercise, or the load used during exercise, to regulate the pressure going through your abdominal wall. It is especially important for women who have been pregnant in the past to reduce the amount or load of activity earlier on in their pregnancy as the linea alba has been stretched before and will fatigue faster compared to women who are pregnant for the first time. Continue exercise and abdominal work, but do not challenge the body to extremes. Recovery is a marathon, not a sprint! Get help from a pelvic health professional Pelvic health specialists strongly recommend women to have their pelvic floor assessed and rehabilitated following childbirth. Professionals like osteopaths, women’s health physiotherapists, pelvic health physiotherapists and clinical Pilates instructors can complete these assessments and prescribe a range of specific exercises and therapeutic techniques to suit your body in its recovery. They also assess the position and movement of your rib cage, spine and pelvis which work together to facilitate optimal contraction of muscle. Seeking help from these professionals will facilitate your body’s natural healing, prepare for optimal results from exercises, and provide relief from pain and discomfort. Further recommendations on managing incontinence and DR include:
C-section scars and stretch marks: may contribute to mild pelvic discomfort In Australia, approximately 36% of women giving birth deliver through caesarean section (C-section). Before we discuss the residual scarring following a C-section, let’s talk about fascia. Fascia is often described as the glad wrap of the body, as it forms a covering over our muscles and creates a smooth pathway for vessels to travel through. Fascia is an important structure in the abdomen, where it holds organs in place and allows them to move freely. When we have scars anywhere in our abdomen, pelvis or even our back, the fascia can become tight and pull organs in different directions making them less movable. This may be interpreted in the body as pain, restricted movement, and a reduction in overall function. Thankfully, the body possesses extraordinary self-healing properties that can work to reduce fascial pulling that occurs with scarring, and aid recovery. Osteopaths use hands on therapy to treat scarring from C-sections and other surgical procedures frequently. One of the best things about scar tissue recovery is that some techniques can be done by yourself. Anytime. Anywhere. If you live with family or friends, you can even teach them to apply these techniques for you (less work for you, more fun for them). Scar tissue massage is easy to learn and may deliver great results with a little bit of commitment. Here are three ways you can begin your scar tissue massage:
Exercise during pregnancy Physical and mental health are key to a positive pregnancy and post-partum experience. Participating in regular, moderate intensity exercise is recommended during all stages of pregnancy for reasons which include:
 Mind health The emotions tied to pregnancy and post-partum recovery can be overwhelming and difficult to manage. Connecting with people you trust is a great way to build a supportive network. One in five expectant women and one in ten expectant men experience anxiety and/or depression during pregnancy and in the first years of parenthood, which is why organisations like Perinatal Anxiety and Depression Australia (PANDA) have been established. PANDA offers Australians a National Helpline and other resources that can be found on their website to aid recovery. Their helpline is available on 1300 726 306 Monday-Friday, 9am-7:30pm (AEST). The PANDA website may be accessed through this link PANDA - Perinatal Anxiety & Depression Australia Other local businesses that may be helpful during the pregnancy and post-partum period: Secrets from the Honey Tree Secrets from the Honey Tree – Eumundi Traditional Health and Healing Centre located in Eumundi Pelvic health Physiotherapist, such as Pre and Postnatal Care (alchemyinmotion.com.au) located in Noosa
1 Comment
|
HMC TEAMIf you find something of interest that might suit this space, or would like information on a specific topic, let us know at [email protected]
Archives
December 2023
Categories |

 RSS Feed
RSS Feed
