 By Kirby Edwards Why would a teenager need to see an osteopath? Osteopathy for teenagers looks at structure, function and movement in relation to everything else. We look at those complex relationships through the body, including the bones of the head, pelvis, limbs and torso. As we transition through puberty, it can be a challenging time. A lot of changing hormones (and heightened emotions), challenging environments, growth spurts and often compounding injuries of falls and traumas from adolescence.Before we put our hands on, we will talk to the teen and the parents about the birth and pregnancy, medical history including any allergies, falls, broken bones and family history, sleep patterns to gain as much information as we can. We might even ask about your bowel movements or menstruation (horrified gasp!)  How do you treat a teenager? As osteopaths, we have a variety of tools in our toolkit for treatments and often use a combination. We may use cranial osteopathy or biodynamics, which is a gentler approach that helps the body to find better balance optimise movement. We may use soft tissue techniques such as massage, muscle tension release or stretching. Other techniques we may perform include joint mobilisation, muscle energy techniques or myofascial techniques. Education and advice to manage your condition between appointments is often provided, as well as some take home exercises. What can an osteopath do for teenager? Osteopaths can support teenagers with a variety of issues:
 What can I expect post treatment? As with any treatment for anyone, there is an adjustment period to the new balanced normal. Each person can react differently. It can take between 1-3 days to settle down, although for some may settle down straight away. Feel free to give us a call if you have any questions. We may also send you off with a referral to a GP or another specialist if the issue is out of our scope.
0 Comments
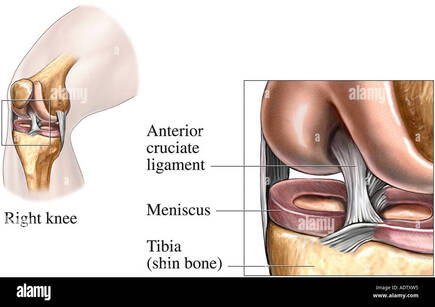 By Liam Neyland What is the ACL The anterior cruciate ligament (ACL) is a dense band-like connective tissue designed to attach the bottom of the femur to the top of the tibia. The ACL is one of the major structural aspects of the knee, it’s main function to resist rotational loads and anterior tibial translation (stop the shin bone falling forward). Despite being only one of the four major ligamentous structures of the knee, injury to the ACL is one of the most common knee injuries in Australian sport. It is so common in Australia that we lead the world in reported ACL injuries, with an increase of 70% in the last 15 years according to studies. Between 2000 and 2015 a reported 200 000 ACL reconstruction surgeries were performed which on average has an annual cost of 142 million a year to the medical system.  How does an injury occur? Despite the fact that the most common demographic who suffer from ACL injuries are young athletes in contact sports , the majority of injuries are non contact in nature. Approximately 70% of all ACL injuries are non contact with most occurring from a plant and pivot motion. The ACL is put under further stress if these movements are performed during rapid deceleration into acceleration. Females are 3 times more likely to have an ACL injury for a number of reasons, including ligament laxity. The severity of an ACL injury is classified into 3 separate grades; grade 1 is a stretched ligament without any tears occurring, grade 2 is a partial tear and a grade 3 is a full tear.  How is it diagnosed? Most ACL injuries can be diagnosed from a comprehensive history taking and physical examination, which can be performed either by a GP or by a manual therapist like an Osteopath. The examination would include a few orthopaedic tests that are designed to stress the ACL to determine how much laxity is present or if the ACL is still intact. A GP or manual therapist may refer for extra tests such as an MRI, x-ray or ultrasound for confirmation of the diagnosis or if they suspect other structures of the knee may be damaged as well which is common with most ACL injuries.  How can an Osteopath help? The severity of the ACL injury will be the main factor in determining what treatment approach may take place. For low level injuries the use of manual techniques such as articulation, contraction/relaxation and soft tissue work may be used to reduce inflammation and decrease overall pain. For a higher level injury, including full ruptures, the treatment approach may differ as an ACL reconstruction may be required. If surgery is not warranted by a specialist or not preferred by the patient then treatment would involve the implementation of an exercise and rehabilitation program which may focus on prevention of further injury. These programs may be designed to strengthen muscles that may have been a driving force for the original injury or to correct poor mechanical movement and alignment of the knee as well as other major joints of the body. If surgery has already been performed a rehabilitation program can still be used for treatment with the main goal focusing on return to sport or work. If you are suffering from an ACL injury, the Osteopaths at HMC Osteopaths are happy to help using their knowledge and experience with treating several different sporting injuries. References Increasing rates of anterior cruciate ligament reconstruction in young Australians, 2000-2015 - PubMed (nih.gov) ACL injury - Diagnosis and treatment - Mayo Clinic The biomechanics of ACL injury: progresses toward prophylactic strategies - PubMed (nih.gov) Anterior Cruciate Ligament (ACL) Injury - Physiopedia (physio-pedia.com) |
HMC TEAMIf you find something of interest that might suit this space, or would like information on a specific topic, let us know at [email protected]
Archives
December 2023
Categories |

 RSS Feed
RSS Feed
