 By Liam Neyland What is Dry needling? Dry needling is a form of treatment modality that many health professionals implement. It involves the use of a sterile “dry” single use needle being inserted into the skin and muscle. This particular technique is aimed toward myofascial trigger points that are found in muscles. These trigger points are normally found as hypersensitive and or palpable nodules. The overall goal of dry needling is to help reduce muscle pain and or spams, increase surrounding tissue range of motion and improve nerve conductivity. How does it work? The way that this treatment works can be quite complex in nature. In the most simple explanation when these trigger points are stimulated through the use of the needle, a ‘twitch’ like response is produced in the muscle fibres. This stimulation creates a local influx of blood products such as red blood cells to the affected area. This influx is part of the natural inflammation process which in turn helps stabilise and strengthen surrounding connective tissue. During this process the nerve that innervates the target muscle is also stimulated resulting in nerve fibers releasing specific chemicals that interrupt pain signals which in turn causes muscle depolarisation and relaxation from previously tightened states. What can it be used to treat? Dry needling can be used to treat a multitude of conditions. Ranging from but not limited to tendinitis, headaches, general muscle aches/pains and acute soft tissue injuries. Dry needling will only be a small portion of the treatment consultation as your osteopath will utilise a number of other treatment techniques to best maximise the healing time frame. During treatment of certain conditions having dry needling can be sore during or post but this is normally a case to case basis with most patient’s not feeling any pain or discomfort due to how thin the needle is 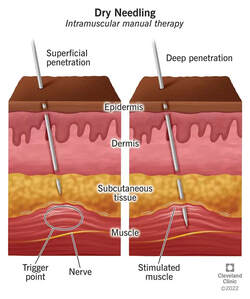 Is it the same as acupuncture? Dry needling and acupuncture have lot’s of similarities between the two. With both inserting needles into specific parts of the body. However, dry needling is used in a more localised fashion where the muscle or region is being treated not the entire body. What Would I expect During treatment? During a usual treatment session you will be placed in a comfortable position dependent on what area is being targeted whether it be seated or lying down on either your stomach or back. Once settled a needle will be gently inserted into the trigger point, once in depending on the expected outcome the needle will either be dynamically utilised (moving needle) or statically utilised (stays still). The needles will only be inserted for 30 seconds to 7 minutes depending on a variety of factors. If you believe that dry needling may be beneficial for you or if you have any questions regarding the procedure, the staff at HMC Osteopath’s are more then happy to answer any questions you may have. Reference Dry needling: a literature review with implications for clinical practice guidelines - PMC (nih.gov) Dry needling - Physiopedia (physio-pedia.com) The effectiveness of superficial versus deep dry needling or acupuncture for reducing pain and disability in individuals with spine-related painful conditions: a systematic review with meta-analysis - PMC (nih.gov)
1 Comment
By Ramona Packham Who better to learn about menopause and the impact it has on one’s life than from those going through it themselves? Read on to discover insights into three women’s experiences through menopause. One of my personal take home messages is how different one person’s experience can be from another! QUESTION 1# Please state your age and stage of menopause (i.e. perimenopausal, menopausal). If menopausal, how long have you been going through this? What age did you become perimenopausal or menopausal? Person 1.
QUESTION 2# Please state 3 of your main symptoms, and a short summary of how each one has affected your life. You can mention how these symptoms might have contributed to other symptoms. Person 1.
All these tend to affect each other and of course changes to life. I choose breathable clothing, do Pilates, exercise each day, take caffeine and hydrated sticks in water to give me energy to get through the day as tired from not sleeping well. Person 2. Only one symptom, which was very slight hot flashes that lasted for a minute or two. Person 3. Hot flushes in the legs. Mood swings. Weight gain and slowed metabolism. Person 4.
 QUESTION 3# Do you suffer from headaches or migraines? If so:
Person 1. I do suffer from headaches. I generally know why I get them which are following: My vision: I wear glasses and often find if too much glare or sun or night-time where I have to really concentrate can bring on a headache. I can’t read too much or look at screen as I can get a headache. I have two different eye visions. Lack of Sleep: tired from not sleeping well due to going to toilet or just waking up for no reason. This can lead to wrong position when I do sleep leading to sore neck muscles. Dehydration: Particularly when I am at work I may not get to drink enough water. Driving to my dad to look after him: whether it is tension, anxiousness, or stress or whether it’s a long way driving that I am not sure. My sister also experiences this. Strategies:
Person 2. No, extremely rare. If I did get a headache I don’t think it was related to menopause. Sleep and or relax rest helped with rare headache. Person 3. So far, I don’t suffer from migraines so can’t answer any of these questions. Person 4.
QUESTION 4# Do you exercise? If so, what exercise do you do and how often? Has this changed since becoming menopausal? Person 1. Yes I exercise. I have always enjoyed outdoors walking, hiking, cycling. Average: 5/7 days a week. Walk (5km average) 4x Walk up steps 2.5km then return (You Yangs hike) 1x (sometimes 2 x) Pilates 2x Since menopause I started Pilates to help strengthen muscles as well as help with some extra aches and pains (age or menopause not sure). Person 2. Yes, some stretching muscle exercisers and occasional walking, at least 2/3 times a week. It has not really changed but sometimes less or more. Person 3. I walk at times, sometimes hike. I have a job that keeps me active. I used to walk more but I get so tired after work now. Person 4. Minimal Walking, short HIIT routines QUESTION 5# What was your main concern in lead up to perimenopause if you had any. How has this concern been addressed? Do you still have any fears around the changes associated with menopause? Person 1. I did not have many concerns basically as my last 15yrs has been dedicated to caring for my parents as well as bringing up my girls that I simply didn’t think much of myself. This probably helped as I wasn’t concerned. I have Faith in God which helps me regarding my health. I know He knows everything about my life which is comforting that I am not alone. Person 2. No concerns or fears, although my mother had medium to extreme sudden hot flashes of sweat. Person 3. No concerns really as it was inevitable. I’m worried when I’m through menopause that I will age faster than I am expecting to. Person 4. Later than average age has higher incidence of cancers (familial history of cancer) QUESTION 6# How long were the periods of amenorrhea in your perimenopausal stage? Person 1. Periods were not lasting 4 days like usual. Periods lasted a day towards fully transitioning to menopause to just spotting. They were not once a month, and I didn’t know when they would come and go. Basically over 3 to 4 years reduced in duration and time. Person 2. Period flows lasted less days and lighter and skipped random months. Sometimes no period flow for three months and there was no consistency. On rare occasions period flows were heavier than usual and sometimes lasted longer days, but this occurred only about three times. At 50 years old menopause started and lasted about two years, then the third year I had no periods for at least 12 months, when suddenly I got a heavy period for about two hours in one day and then nothing, and I haven’t had a period since. I visited the doctor and all tests showed that everything was fine. I also discussed my concern with a friend from work who reassured me it was normal to get a random period after a year, it happened to a few people she knew. Person 3. I have continued to have light periods. I had uncontrollable bleeding at 51 and had to seek medical attention. Person 4. 10 days maximum QUESTION 7# Can you provide information to any services, products, or advice that has been personally effective for you in coping with menopausal symptoms? Please list specifics. Person 1. Exercising Daily: I feel this has improved many of my symptoms. My hot flushes are not as frequent, my whole body feels stronger, and I feel better getting out into nature. Arbonne Energy Fizz Sticks: Flavours are great, boosts energy levels (don’t need caffeine however I enjoy a coffee). Energy Renew Gundry: Great Energy and overall health. Skin feels better. Colloidal Silver: helped with any urinary discomfort. Whether itchiness, dryness or burning sensation. Person 2. I noticed my very slight hot flushes occurred when l ate lots of sweets/cakes. The hot flushes never intensified just occurred slight hot flushes. As usual. I reduced my sweets and hot flushes were rare and if occurred were very mild, for a minute or less. Person 3. Have never been given advice on how to cope. Person 4. QUESTION 8# Did you feel prepared for menopause? Person 1. Not really but then I wasn’t really thinking too much about it. I had very difficult periods, heavy bleeding and much discomfort so it was more of a welcome in my life. Person 2. It seemed to happen naturally, yes, l was expecting it at some point in my fifties. Person 3. I accept it as inevitable.  QUESTION 9# Do you discuss your symptoms with other women? Person 1. Not hugely but I have a dear friend who shared how she felt. I would also hear others talking about it. Person 2. Yes, with women friends at work and a couple of close friends. Person 3. Sometimes with good friends. Person 4. Yes QUESTION 10# In your opinion, is there anything lacking in the healthcare system today to help women through these years? Person 1. Yes, lack of education and information from the healthcare system, or school. It seems to come across as a private subject or something and therefore many women do not know about it. I have not come across much information regarding menopause. Information on what you could do to prepare would be helpful to many such as exercise, dietary, meditative areas. Doctors rarely talk about it (mine has not). I also have been to osteopath (s) for different ailments not once has menopause come up as a possible reason for soreness, aches, pains etc. Person 2. Independent research not related or controlled or sponsored by big companies... This ensures accurate science results from independent doctors. More knowledge of natural and healthy options, such as essential oils, herbs, pure foods, exercises to help women rather than drugs or medications that usually have side effects and only treat the symptoms (surface issues) and not the cause. More awareness and information about the triggers and impact of certain supermarket food ingredients, diets, medications taken for long periods of time, etc. Person 3. I don’t think it’s approached by drs very effectively. They should ask more about what’s happening. I had to have an IUD put in to control the bleeding but I’d never heard of it happening to anyone before. The other option is uterine ablation which sounds horrific. Person 4. General information including definitions and non-pharmaceutical methods of assistance. QUESTION 11# Do you have any advice for young women who are getting close to the perimenopausal phase? Person 1. It would be good to share with young women common symptoms to expect in the lead up to menopause so that they are aware that their lives will be affected by the change and that it is normal. I know someone that reached menopause at age 38. She had no idea and had delayed having kids. Good for all women to be aware that it will happen at some point. Person 2. Do not be concerned if your mother has had a difficult menopause. Take notice of what you eat. No refined foods, and eat more unrefined. Be aware of certain chemicals placed in supermarket foods such as preservatives, additives and flavour enhancers. Book to read: The Chemical Maze, guide to food and cosmetic ingredients. Be aware of chemical cosmetic ingredients since it is placed on face near eyes, mouth, nose, brain etc. Choose natural and pure face products. Rest, sleep at least 8 hours, exercise-walking, drink water and or herbal teas, but no soft drinks and alcohol or only on extreme rare occasions. Do not smoke. Regular visits to detox in a sauna, very healthy. Person 3. Don’t be afraid and try to take care of yourself. Please use this space to make any further comments. The floor is yours! Person 1. Pilates has been very helpful to me. My daughter who is an osteopath recommended it. Getting the message regarding Pilates being the perfect exercise for premenopausal and menopausal women – balance, flexibility, muscle strength, women getting together and chatting about their health etc. I had a difficult time since a young teenager with my periods. I experienced a lot of pain, bleeding, not feeling great etc so in away for me to not have to deal with this has given me a break. Person 2. I had an easy menopause, so l shared my lifestyle over years of growing. My sister who smoked from a teenager to 48years old had extreme menopause headaches that lasted for at least 3 days but I don’t know if smoking had any impact. My mother had extreme hot flushes and is over weight. She eats healthy but enjoys her sweets. Person 3. I wish I’d know more about the way menopause varies for each woman. My new dr assures me I’m normal – I’m nearly 56, I should be done with this by now but I’m not. It’s very disconcerting! Wrap up This brings you to the end of this little survey. While the basic physiology of menopause is similar in all women, it is worth noting that everyone’s experience is unique to them. Let’s use this opportunity to encourage women about to go through the menopausal transition, those in it and those beyond it, to look after yourselves. Take this opportunity to reset and make any health-related changes or improvements to set you up for strength in the future. Sharing about your experiences with other women can also be beneficial to both the one sharing, and those who have the pleasure of listening. You never know what someone might relate to. Finally, if anyone reading this has any questions on the topic of menopause, be it personal or generic, please reach out to the HMC Osteopaths team who are here ready to listen and help. By Ramona Packham Since all humans housing functional female reproductive organs go through a transitional stage in their reproductive lives called menopause, it’s a subject beckoning to be discussed. This first blog aims to empower the reader with knowledge by providing a brief introduction to menopause including information on important terms, some basic physiological changes that take place during menopause and common symptoms consequential to these. This blog will be followed by a meaningful post revealing insight into a small sample of women and their experience with menopause. Basic physiology of Menopause Categories explained: Menopause: The final menstrual period which usually occurs between the ages of 45 and 55, with the average onset at 51 years of age. During menopause the body stops producing cyclical oestrogen and progesterone (reproductive hormones) due to loss of ovarian follicles (little sacs within the ovaries that house unfertilised eggs), follicular development, and ovulation (release of the unfertilised egg). Perimenopause: Also referred to as the menopausal transition, is the time preceding until one year following the menopause. Typical characteristics accompanying perimenopause include hormonal fluctuation, anovulatory cycles (the ovary does not release an egg, so ovulation does not occur), irregular menstrual cycles, and the onset of menopausal symptoms. This transition usually lasts between 2-6 years. Post-menopausal: A woman is considered post-menopausal when she has had 12 consecutive months without having her menstrual cycle. Early menopause: The onset of menopause between the ages of 40 and 45. Premature menopause: Also referred to as ovarian insufficiency, is considered if the final menstrual period occurs before age 40. Reasons behind premature menopause include natural cessation of ovarian function, surgical removal of the ovaries, or previous chemo / radiotherapy.  Why the change? The reproductive cycle is regulated by hormones. The amount of each hormone produced changes throughout each menstrual cycle, and across the reproductive lifespan. Let’s start with the disclaimer that hormones are a rather complicated point of discussion, so let’s be brief and fearless of terms like the ‘hypothalamic-pituitary-ovarian axis’ (HPO axis). The HPO axis is the relationship between the hypothalamus in the brain, the pituitary gland sitting just below it which releases hormones to send to the ovaries, and the ovaries (female reproductive organs) that produce Oestrogen and Progesterone (reproductive hormones). In menopause, the body’s physiology changes which slows and stops the production of oestrogen. Given the various roles oestrogen plays, it is not surprising that many menopausal symptoms arise because of this reduction. Vasomotor changes also occur. WOAH let’s rewind for a second and explain vasomotor symptoms. The term vasomotor refers to the neural control of the constriction and dilation of blood vessels and is regulated by a part of the brain called the vasomotor centre. Symptoms including hot flushes, night sweats and sleep disturbance are examples of vasomotor symptoms. Sleep deprivation or reduced sleep quality is also a significant underlying reason for many symptoms of menopause. Sleep deprivation is often tied to vasomotor instability. 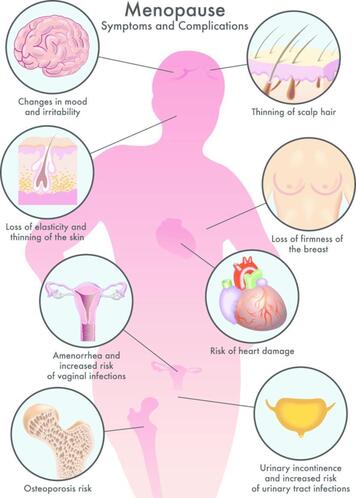 All the wonderful symptoms Symptoms are greatest in the menopausal transition, compared to the post-menopausal stage which is often easier to manage. This is due to the changes in reproductive hormones as explained in the previous section. 80% of women report experiencing menopausal symptoms including hot flushes, night sweats, body aches, breast tenderness, weight gain, dry skin, vaginal dryness, loss of libido, urinary incontinence, and changes in mood and memory. Other less common symptoms can include itchy skin, thinning of the scalp and pubic hair, and skin changes. Symptoms can be classified into two parts:
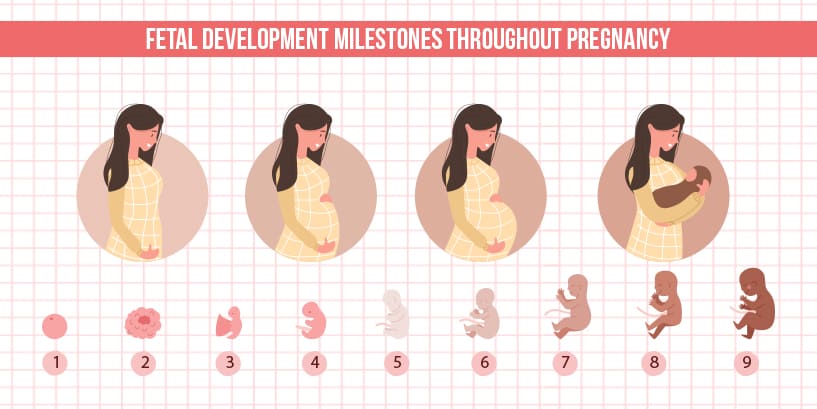
Hot flushes Hot flushes are a hallmark symptom of menopause and are experienced by 75% of women, with approximately 25% of these being significantly problematic. Hot flushes may last 1 to 2 years, however it is not unusual for these to last 10 years or more. A hot flush, as it sounds, is the episodic experience of extreme heat, followed by cutaneous vasodilation and a consequential drop in core body temperature. Women with oestrogen deficiency in the later stages of menopause have a lower than usual thermoneutral zone, which means that even a small increase in core body temperature causes the sensation of extreme heat. Vasodilation (expanding) of blood vessels in the skin and sweating help the body to release heat. Changes in mental status Serotonin is a chemical neurotransmitter that helps to regulate sleep, emotions, and mood, and it decreases by 50% during menopause. Sleep deprivation, depression, anxiety, fatigue, irritability, and loss of libido are all associated symptoms that affect many women as they journey through menopause, especially towards the later stages. While depression does not increase in prevalence among menopausal women compared to other stages of life, it can become apparent in those with a previous history of depression, or because of the presence of other symptoms such as lack of sleep or loss of libido. Some women experience cognitive symptoms like the inability to concentrate and make decisions. Additionally, changes in the menstrual cycle causes unpredictable periods of amenorrhea, or, not having a period, which can be a source of stress and anxiety for many women since it becomes difficult to predict the next period. The vagina Let’s address the elephant in the room and talk about the vagina, and all the changes that go on down there. These symptoms when related to menopause are termed genitourinary syndrome of menopause and are often not spoken about due to discomfort in disclosing this kind of information. Let’s talk about them. Vaginal dryness and dyspareunia (painful sexual intercourse) are two of the most common symptoms experienced by 1/3 women in the later stages of perimenopause, so if you thought you were alone in this boat, you are not. Other symptoms relating to the vagina and structural changes of the vagina that women may observe include burning and irritation of the vagina, decreased lubrication due to changes in vaginal mucous production, thinning of pubic hair, atrophy of the labial fat pad, and resorption of the labia minora. The structural changes of the vagina may be termed as vulvovaginal atrophy. As these symptoms are a result of hormonal change, it is not surprising that hormone therapy is most often the first treatment modality, and for most women the advantages of using hormone therapy outweigh the possible risks. There are always links. Menopausal symptoms have a reciprocal relationship with each other such that one symptom can add to the severity of another. For example, poor sleep can contribute to depressed mood, which can increase one’s perception of discomfort. There is also a link between depressed women experiencing more hot flushes which leads to poorer sleep, particularly as the hot flushes occur nocturnally. So, these vicious cycles go on, not dissimilar to those that influence pain conditions. As this can be very frustrating, it is important to speak about them and seek out management. These profound reproductive and hormonal changes cause 90% of women to seek professional healthcare advice to help them cope with the associated symptoms. Small suggestions The menopausal transition is a great time to think about overall health and wellness and be assessed by a healthcare professional, like a GP, an Osteopath or both! This is prime time to get your body feeling healthy and strong, preparing you for the post-menopausal stages of life. Achieving good cardiovascular fitness and optimal bone density are absolute priorities. Due to cycle irregularity throughout the menopausal transition, continuing contraception is suggested as pregnancy is still possible. It is also worth considering self-care practices throughout the menopausal transition. Making sure you prioritise your health and wellbeing, being gracious to your body and patient with what it is going through, are factors that can have a very positive influence on both physical and mental health. More suggestions from REAL women in the next blog. Stay tuned! Stay tuned for my next blog to learn from women and their experience through the menopausal transition. References Australian Menopause Society. (2017). The perimenopause or menopausal transition. North American Menopause Society (NAMS) - Focused on Providing Physicians, Practitioners & Women Menopause Information, Help & Treatment Insights Australian Menopause Society. (2022). What is menopause? North American Menopause Society (NAMS) - Focused on Providing Physicians, Practitioners & Women Menopause Information, Help & Treatment Insights Australian Menopause Society. (2021). Risks and benefits of menopausal hormone therapy. North American Menopause Society (NAMS) - Focused on Providing Physicians, Practitioners & Women Menopause Information, Help & Treatment Insights By Angus Nicol As the tiny human reaches the end of the peace and comfort of their nine month incubation period, they start to descend, head down facing backwards until it engages behind the pubic bone, in a process known as “lightening”. At the same time, preparing for a traumatic entry for their solo journey upon our planet. Mums cervix softens and becomes thinner in preparation to dilate during labour. Labour begins when the muscles at the top of the uterus contract, initiating the baby’s traumatic journey through the cervix/vagina and out into the real world. Towards the start of labour, the water breaks and the baby is released from the sac of amniotic fluid it called home. The initiation of labour is strongly influenced by the release of oxytocin. 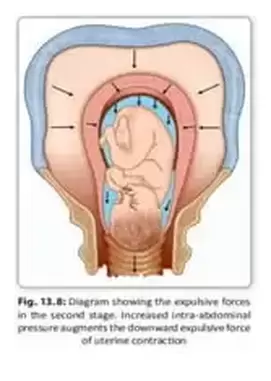 Oxytocin is also known as the “love hormone”, and more recently, the “spirit hormone” because of it’s important role in feeling love and in social interaction. This hormone is also thought to play an integral role in feelings of spirituality by enhancing feelings of interconnectedness. This creates a beautiful juxtaposition - The significance of oxytocin helping to initiate labour, the physical separation of mother from baby, with the love hormone responsible for an eternal emotional bond between parent and child. As labour progresses, the mother’s cervix dilates, creating a tunnel that exits the cavernous womb. Contractions get stronger and stronger, forcing the baby’s head down into the cervix. During this process, the baby’s unfused skull bones are squashed and forced to overlap and take on the shape of an elongated cone with a rounded end. Altogether, labour is a process that can last anywhere from a few hours to a couple of days (average 12-14 hours). 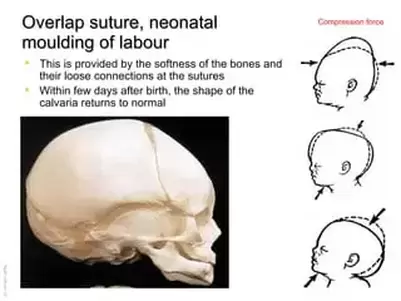 Once the baby’s head passes through the vagina, it usually only takes a few more contractions until the rest of the body is liberated. The newborn may appear blue and mottled. However it should take it’s first breath, creating it’s own life force energy, within the first minute following birth. As the baby continues to breathe, appearance should become pinker as blood and oxygen circulates through the body. The baby will be covered in amniotic fluid which is important for the baby to be able to smell and taste, because it creates a sense of familiarity and security in an otherwise alien environment. Following birth, the placenta will also be delivered, along with the umbilical cord. Often the support person will be invited to cut the cord, signifying the end of the newborns physiological dependence on it’s parent. However, connection via skin-to-skin contact immediately following birth is important as it helps start and sustain breastfeeding, and also aids in the maintenance of baby’s core body temperature (which is basically a measure of energy release via heat). Baby will usually ask for it’s first meal around an hour after birth. The newborn will be exhausted from the traumatic birthing process, so shortly after it has been nourished it will usually fall into a long sleep that may last 6 hours. Usually a baby will spend about half of it’s first day on Earth asleep. Baby has been listening to Mums voice for the last half of pregnancy, and will recognise it when you speak to them after birth - they may also recognise partner/support persons voice if they have also been talking near the womb. This creates a sense of security for the newborn, and they may respond by turning their head towards the voice. Your baby will also be able to hear your heart beating as they did in the womb. A new borns vision is blurred at birth but they will be able to focus on your face from about 30 centimetres away - the ‘cuddle distance’ (roughly distance from Mums breast to face). Your baby will make the connection between what they hear and what they see. 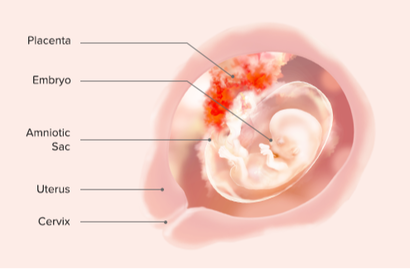 By Angus Nicol First Trimester At a more macro, less cellular level, there are some significant milestones between weeks 3-8. Weeks 4-5 - The heart usually starts beating between 4th-5th weeks and all the muscles and blood vessels in our body branch outwards from our growing, beating heart. Eye pits form, limb buds become apparent, first signs of pulmonary system are formed (connects heart to lungs). Week 6 - Uncontrolled foetal limb movements start to occur, paddle-shaped fingers/toes undergo “apoptosis” (programmed cell death) so webbing disintegrates leaving defined fingers/toes. Week 7 - Facial structure more complex. Includes nostrils, outer ears and lenses. By the end of Week 7, the foetus is distinguishable as a tiny alien-human. Week 8 - Head as large as rest of embryos body, external genitalia become apparent (can’t distinguish M/F), cartilage begins ossification process into bone. Week 10 - Organs like kidneys, intestines, brain, and liver are beginning to function, and fingernails and toenails are starting to form. Week 11 - Red blood cells (carry oxygen vital for energy/life) start forming in liver. By end of week, external genitalia apparent (penis or labia & clitoris). Bud for teeth appear. Now no longer classified as embryo, now classified as foetus. Week 12 - Face has a more developed profile. Second trimester Week 13-16 - Sensory organ development. The eyes move closer together; blinking motions begin, although eyes sealed shut. Lips exhibit sucking motions. Scalp begins to grow hair. The excretory system developing: the kidneys well-formed; meconium (fetal feces) begins to accumulate in the intestines. Weeks 16-20 - Fetus grows & limb movements become more powerful. Mother may begin to feel “quickening” (foetal movements - space restrictions force foetus into foetal position). Skin coated with waxy substance “vernix caseosa) for protection, moisturisation and lubrication during birth. Third trimester Weeks 21–30 - Rapid weight gain (important for maintaining stable body temp after birth). Bone marrow completely takes red blood cell synthesis, nerves undergo myelination (production of fatty protective sheath that helps electrical conduction - this process continues until adolescence). Fetus grows eyelashes. Eyelids not fused (can open/close). Lungs produce surfactant (substance that reduces tension in lungs, assists proper lung expansion after birth). Males: Testes descend into scrotum(towards the end). Fetus at 30 weeks measures 28 cm from crown to rump, exhibits approx body proportions newborn (but much leaner). Baby may begin dreaming (28-32wks). Weeks 31 - Birth - Fetus lays down fat (fills out layer below skin aka “hypodermis”, skin transitions from red/wrinkled to soft/pink. Nails grow to tips of fingers & toes. At birth, average crown-to-rump length is 35.5–40.5cm, weight 2.5–4kg. |
HMC TEAMIf you find something of interest that might suit this space, or would like information on a specific topic, let us know at [email protected]
Archives
December 2023
Categories |

 RSS Feed
RSS Feed
