|
By Ramona Packham Since all humans housing functional female reproductive organs go through a transitional stage in their reproductive lives called menopause, it’s a subject beckoning to be discussed. This first blog aims to empower the reader with knowledge by providing a brief introduction to menopause including information on important terms, some basic physiological changes that take place during menopause and common symptoms consequential to these. This blog will be followed by a meaningful post revealing insight into a small sample of women and their experience with menopause. Basic physiology of Menopause Categories explained: Menopause: The final menstrual period which usually occurs between the ages of 45 and 55, with the average onset at 51 years of age. During menopause the body stops producing cyclical oestrogen and progesterone (reproductive hormones) due to loss of ovarian follicles (little sacs within the ovaries that house unfertilised eggs), follicular development, and ovulation (release of the unfertilised egg). Perimenopause: Also referred to as the menopausal transition, is the time preceding until one year following the menopause. Typical characteristics accompanying perimenopause include hormonal fluctuation, anovulatory cycles (the ovary does not release an egg, so ovulation does not occur), irregular menstrual cycles, and the onset of menopausal symptoms. This transition usually lasts between 2-6 years. Post-menopausal: A woman is considered post-menopausal when she has had 12 consecutive months without having her menstrual cycle. Early menopause: The onset of menopause between the ages of 40 and 45. Premature menopause: Also referred to as ovarian insufficiency, is considered if the final menstrual period occurs before age 40. Reasons behind premature menopause include natural cessation of ovarian function, surgical removal of the ovaries, or previous chemo / radiotherapy.  Why the change? The reproductive cycle is regulated by hormones. The amount of each hormone produced changes throughout each menstrual cycle, and across the reproductive lifespan. Let’s start with the disclaimer that hormones are a rather complicated point of discussion, so let’s be brief and fearless of terms like the ‘hypothalamic-pituitary-ovarian axis’ (HPO axis). The HPO axis is the relationship between the hypothalamus in the brain, the pituitary gland sitting just below it which releases hormones to send to the ovaries, and the ovaries (female reproductive organs) that produce Oestrogen and Progesterone (reproductive hormones). In menopause, the body’s physiology changes which slows and stops the production of oestrogen. Given the various roles oestrogen plays, it is not surprising that many menopausal symptoms arise because of this reduction. Vasomotor changes also occur. WOAH let’s rewind for a second and explain vasomotor symptoms. The term vasomotor refers to the neural control of the constriction and dilation of blood vessels and is regulated by a part of the brain called the vasomotor centre. Symptoms including hot flushes, night sweats and sleep disturbance are examples of vasomotor symptoms. Sleep deprivation or reduced sleep quality is also a significant underlying reason for many symptoms of menopause. Sleep deprivation is often tied to vasomotor instability. 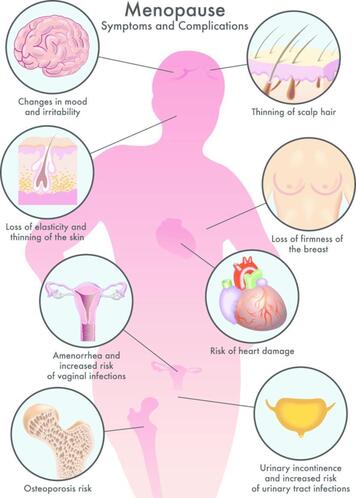 All the wonderful symptoms Symptoms are greatest in the menopausal transition, compared to the post-menopausal stage which is often easier to manage. This is due to the changes in reproductive hormones as explained in the previous section. 80% of women report experiencing menopausal symptoms including hot flushes, night sweats, body aches, breast tenderness, weight gain, dry skin, vaginal dryness, loss of libido, urinary incontinence, and changes in mood and memory. Other less common symptoms can include itchy skin, thinning of the scalp and pubic hair, and skin changes. Symptoms can be classified into two parts:
Hot flushes Hot flushes are a hallmark symptom of menopause and are experienced by 75% of women, with approximately 25% of these being significantly problematic. Hot flushes may last 1 to 2 years, however it is not unusual for these to last 10 years or more. A hot flush, as it sounds, is the episodic experience of extreme heat, followed by cutaneous vasodilation and a consequential drop in core body temperature. Women with oestrogen deficiency in the later stages of menopause have a lower than usual thermoneutral zone, which means that even a small increase in core body temperature causes the sensation of extreme heat. Vasodilation (expanding) of blood vessels in the skin and sweating help the body to release heat. Changes in mental status Serotonin is a chemical neurotransmitter that helps to regulate sleep, emotions, and mood, and it decreases by 50% during menopause. Sleep deprivation, depression, anxiety, fatigue, irritability, and loss of libido are all associated symptoms that affect many women as they journey through menopause, especially towards the later stages. While depression does not increase in prevalence among menopausal women compared to other stages of life, it can become apparent in those with a previous history of depression, or because of the presence of other symptoms such as lack of sleep or loss of libido. Some women experience cognitive symptoms like the inability to concentrate and make decisions. Additionally, changes in the menstrual cycle causes unpredictable periods of amenorrhea, or, not having a period, which can be a source of stress and anxiety for many women since it becomes difficult to predict the next period. The vagina Let’s address the elephant in the room and talk about the vagina, and all the changes that go on down there. These symptoms when related to menopause are termed genitourinary syndrome of menopause and are often not spoken about due to discomfort in disclosing this kind of information. Let’s talk about them. Vaginal dryness and dyspareunia (painful sexual intercourse) are two of the most common symptoms experienced by 1/3 women in the later stages of perimenopause, so if you thought you were alone in this boat, you are not. Other symptoms relating to the vagina and structural changes of the vagina that women may observe include burning and irritation of the vagina, decreased lubrication due to changes in vaginal mucous production, thinning of pubic hair, atrophy of the labial fat pad, and resorption of the labia minora. The structural changes of the vagina may be termed as vulvovaginal atrophy. As these symptoms are a result of hormonal change, it is not surprising that hormone therapy is most often the first treatment modality, and for most women the advantages of using hormone therapy outweigh the possible risks. There are always links. Menopausal symptoms have a reciprocal relationship with each other such that one symptom can add to the severity of another. For example, poor sleep can contribute to depressed mood, which can increase one’s perception of discomfort. There is also a link between depressed women experiencing more hot flushes which leads to poorer sleep, particularly as the hot flushes occur nocturnally. So, these vicious cycles go on, not dissimilar to those that influence pain conditions. As this can be very frustrating, it is important to speak about them and seek out management. These profound reproductive and hormonal changes cause 90% of women to seek professional healthcare advice to help them cope with the associated symptoms. Small suggestions The menopausal transition is a great time to think about overall health and wellness and be assessed by a healthcare professional, like a GP, an Osteopath or both! This is prime time to get your body feeling healthy and strong, preparing you for the post-menopausal stages of life. Achieving good cardiovascular fitness and optimal bone density are absolute priorities. Due to cycle irregularity throughout the menopausal transition, continuing contraception is suggested as pregnancy is still possible. It is also worth considering self-care practices throughout the menopausal transition. Making sure you prioritise your health and wellbeing, being gracious to your body and patient with what it is going through, are factors that can have a very positive influence on both physical and mental health. More suggestions from REAL women in the next blog. Stay tuned! Stay tuned for my next blog to learn from women and their experience through the menopausal transition. References Australian Menopause Society. (2017). The perimenopause or menopausal transition. North American Menopause Society (NAMS) - Focused on Providing Physicians, Practitioners & Women Menopause Information, Help & Treatment Insights Australian Menopause Society. (2022). What is menopause? North American Menopause Society (NAMS) - Focused on Providing Physicians, Practitioners & Women Menopause Information, Help & Treatment Insights Australian Menopause Society. (2021). Risks and benefits of menopausal hormone therapy. North American Menopause Society (NAMS) - Focused on Providing Physicians, Practitioners & Women Menopause Information, Help & Treatment Insights
0 Comments
Leave a Reply. |
HMC TEAMIf you find something of interest that might suit this space, or would like information on a specific topic, let us know at [email protected]
Archives
December 2023
Categories |

 RSS Feed
RSS Feed
