 By Kirby Edwards What would a child need to see an osteopath? Children are very resilient and often bounce back from injuries quite well. However, sometimes problems earlier in life can lead to discomfort later on. This may include postural issues, movement, breathing, overall development and re-occurring infections. We aim to release any tension or strains in the tissues to prevent any compensatory changes throughout their prime growing time. What can an osteopath do for older children and toddlers? Osteopaths can assist with:
As the children transition from adolescent to teenage years – traumas that the child may have experienced can become more obvious with the influence of hormones and onset of puberty. Some of the changes that you may notice include scoliosis, headaches, poor concentration, brain fog. How do you treat a child? Before we begin hands-on therapy, we will talk to the parents about the pregnancy, birth, medical history of the baby and family, feeding and digestion, sleep patterns and movements of the baby to gain as much information as we can as well as answer any questions you have. When we place our hands on, we will assess how the body is generally moving, respiration, movement of the cranial bones of the skull and specific muscle or joint issues. We will then discuss a treatment plan which may include some referrals, homework or exercises as well as potentially some lifestyle or diet changes. The treatment will depend on what the child/toddler presents with, their personality and what age they are. There may be a gentler approach – similar to the one we have with babies where we avoid any sharp manipulations or firm treatment and approach the toddler or child using cranial osteopathy or working with the fluid dynamics of the body to release any tissues that are under tension and restore optimal balance. If they are a little older, we may use some other techniques such as METs (muscle energy techniques) or other techniques which we will discuss with the child and parent before performing.  What is cranial osteopathy? This is a gentle hands-on treatment that helps the body to find better balance and optimise movement. Osteopaths are trained to develop their palpation skills. With Osteopathy in the Cranial Field (OCF) we are trained to feel subtle motion in the whole body. This is called the Primary Respiratory Mechanism (PRM). Although the name is ‘cranial,’ this mechanism can be felt and worked on from anywhere in the body. One of the principles of Osteopathy is that it is all connected. Osteopaths see connections between different parts of the body and by working with this principle aim to optimise the body’s function. OCF is a subtle refined approach that can affect all systems of the body aiming to restore balance and health. Cranial Osteopathy can be of benefit for everyone, but due to its gentle effective approach is ideal for babies and children. What can I expect post treatment? As with any treatment for anyone, there is an adjustment period to the new balanced normal. Each toddler or child (any person) can react differently, but often they are very sleepy, hungry or maybe a little agitated. It can take between 1-3 days to settle down, although for some may settle down straight away. Feel free to give us a call if you have any questions. Some injuries/traumas may need to be assessed by the emergency or a doctor. After serious illness or injury has been excluded, Osteopathy may be able to assist to get your child back on track. If your child has had a trauma and has any of the following:
Please take your child to emergency or a doctor. Some things are out of the scope of Osteopathy and need medical attention as soon as possible.
0 Comments
Sit up straight! Improving work ergonomics to decrease pain, increase energy & productivity23/3/2022 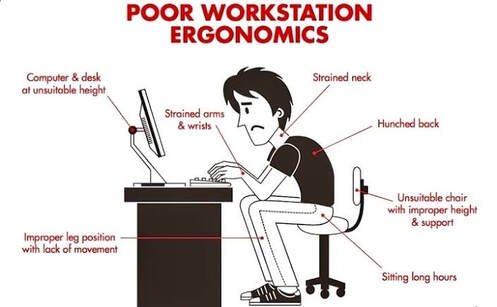 By Angus Nicol Slouchy slouch - How are you sitting? Ever heard of the saying “sitting is the new smoking?” As the health conscious reader I know you are (since you’re reading this blog), I’m almost sure you have. And it’s true, prolonged periods of “sedentary” behaviour (physical inactivity) over long periods can have detrimental effects on both your physical and mental health. This is worrying, since an estimated 81% of Australians work in occupations that require some sitting, with over half of Australians reporting that they sit for work “all the time” or “often”. Today I’m not here to lecture you about all the health consequences of sitting (that may have to wait for another time), but rather to give you some hints and tips about proper desk posture and ergonomics - so that when you are sitting, at least you’re doing it in the healthiest possible way! I feel this is becoming increasingly important given that there are more people than ever working from home in less than ideal workspaces (whether that be in bed/on the couch, at the kitchen table etc). I’m sure you would all recognise the classic “desk posture”. Generally what you will see is four basic characteristics in the upper body:
This happens because when we’re sitting at a desk, everything we need is in front of us, so we slouch to get closer to it. This causes the muscles in the front of our chest to become short and tight and holds us in this rounded shoulder position. The opposite happens to the muscles in our back, over a long period of time the muscles between our spine and our shoulderblades may get weak and lazy, and they may no longer have the strength or endurance to hold our shoulders backwards. This contributes to the upper part of the back becoming increasingly rounded and stiff, making it hard to sit up tall. This means that to continue looking straight ahead, you have to tilt your head backwards slightly. This requires excessive use of the muscles in the base of your skull and back of your neck and they may then become tight and give you neck pain. These muscles also refer up towards your skull, so tightness in these muscles may also be responsible for headaches! I feel it’s important to note that stress commonly causes these muscles to become tense, and exacerbate your neck pain and headaches. Have a look in the mirror - look front-on and side-on, and notice the position of your shoulders, the curve in your upper back and the position of your neck. Does any of it fit what I just described? Well fear not, you’re not alone. This is one of, if not, THE most common complaint I see in practice… but the good news? YOU CAN DO SOMETHING ABOUT IT!  Ergonomics 101 - The quick fixes A good place to start is by checking your work/desk setup… because if this isn’t ideal, chances are you’re going to be fighting an uphill battle. Where possible (and I know it may not always be!), try to have a dedicated area that you work from if working from home. Try to avoid sitting on surfaces that are too soft (eg beds or soft couches), as these are sacred bits of furniture that should be used for relaxation and enjoyment purposes only! Not to mention they are a posture nightmare! Here are some tips to try and ensure good posture when sitting at your desk. If possible, read this next part at your desk, and make adjustments as you go. It should only take a couple of minutes, and could save you a lot of pain and discomfort!
 Need some help? Here are some people and gadgets to assist you. Okay, how are you feeling now? Although it may seem relatively straightforward, getting this right can be a bit tricky. Sometimes some problem-solving, a bit of imagination and a helping hand is necessary. So, if you’re still struggling to achieve an ideal desk setup, it might be time to try to enlist some help. There’s a few ways you can go about this! First of all, take a photo of your current desk setup (ideally from side on with you sitting in it) and bring it into your local osteopath! We may be able to offer tailor-made advice and recommendations to perfect your desk setup. Other healthcare practitioners such as physiotherapists, chiropractors, GPs and occupational therapists (OTs) may also be able to offer sound advice! Furthermore, there is an overwhelming amount of gizmos and gadgets out there designed to help improve your work ergonomics and make you as comfortable as possible. There is anything from ergonomically designed seats, sit-to-stand desks, ergonomic mouses and keyboards, footstools, back braces and much more! However, not all of these may be necessary for you, and there are some dodgy ones out there, so I highly recommend consulting your local healthcare practitioner to assess what may be useful for you, before wasting money on expensive fancy and potentially unnecessary things! Another little hot tip… many large corporations (and even some small-medium organisations) employ professionals to perform ergonomic assessments, so it may be well worth your while and a good excuse to stand up and go for a wander to HR, or to your managers office, and ask if they can get someone to inspect for you. Sometimes workplaces are willing to cover expenses for any equipment that you require too! Because after all, happy, pain-free employees are likely to be more productive and make them more money… so your comfort is in their best interests too!  Visit your osteo! Great! So now you have a perfect desk setup. But wait… there’s more. Think about your current job, and previous jobs before that. Do you think you could calculate the time spent sitting (probably with poor posture)? Guess what, a new desk setup isn’t magically going to reverse years of poor posture! BUT some hands-on treatment and some simple, easy exercises may help. Osteopaths can assess the main cause of your pain/discomfort and provide manual therapy and personalised exercises to help alleviate your pain, headaches and improve your posture! We may also take into account any other factors that may be influencing your pain (eg stress levels, diet & sleep etc). However, from a purely biomechanical perspective, an osteopaths goals may include:
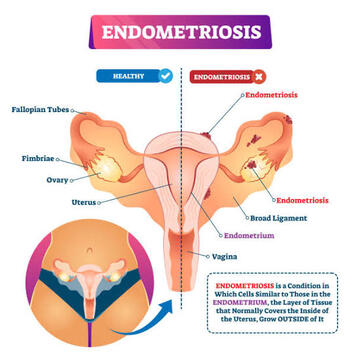
Most of the time, postural complaints are not something that can be fixed instantly. Things that have been there for a long period of time often take a while to resolve. However, with a little bit of hands-on treatment and some dedication to rehabilitation exercises, you can see significant improvements in pain and headaches within 2-8 weeks… which is not long considering how long it may have been an issue for! Please see below for a few easy exercises you can do whilst at your desk, however this is just the tip of the iceberg, come and see us for a more personalised and comprehensive approach tailored just for you! By Liam Neyland As march is Endometriosis awareness month, we at HMC Osteopath’s thought it would be a great time to share some helpful information about this condition. What is Endometriosis? A fair few of you may be wondering what exactly is Endometriosis? Despite the condition affecting approximately 1 in 9 women before they hit their 40’s in Australia, it is a relatively unknown condition within the public. Simply put endometriosis is when cells (endometrium) that usually line the cavity of the uterus, better known as the womb, grow in other parts of the body. These cells can occur at almost any site within the pelvis, but is most commonly found to be sitting on the peritoneum of the pelvis, behind the vagina and uterus, underneath the ovaries and sometimes on the ovaries themselves. In it’s more severe forms this condition can even grow inside the Fallopian tubes or even within the ovary itself. However, there have been cases where these cells have been found outside the pelvis like for example the lungs (thankfully these cases are extremely rare). Despite the fact these cells are not present in the uterus they still respond to hormonal messages from the ovaries. This is especially true during the menstruation period of a women’s cycle, as these cells will bleed every month resulting in inflammation, scarring and in some cases organs to stick together. It is for this reason why women suffering from endometriosis can have such debilitating pain. Along with debilitating pain the disease can affect fertility. How does Endometriosis affect Fertility? The link between fertility and endometriosis is unfortunately unclear, however the stage of the condition and location do play a major role on possible fertility issues. Examples of this are if extensive scarring within the pelvis could result in pain during intercourse, lowering a women’s enjoyment and or dreading the act of intercourse as a whole. Another example would be the Fallopian tubes could become tangled in the scar tissue limiting it’s ability to safely transfer the egg from the ovary to the womb. These are two of many possible outcomes that endometriosis can effect a women’s fertility. Thankfully, many women with this condition can still become pregnant as an estimated 70% of women with mild to moderate endometriosis get pregnant without the use of external treatment. 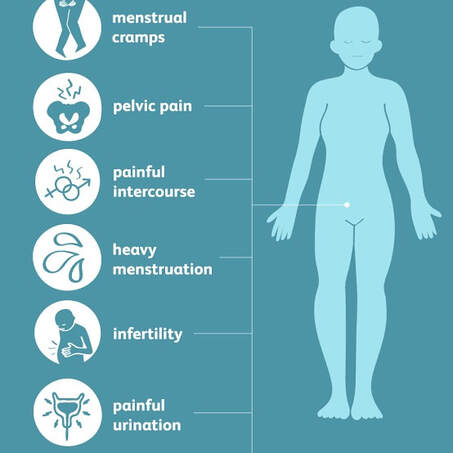 What are the Symptoms of Endometriosis? The symptoms that women experience while suffering from endometriosis will be different by a case to case matter. As the severity of the condition does not necessarily coincide with the symptoms felt but instead where the lesions are located. Common Symptoms include:
What causes Endometriosis? Currently there is no known cause of endometriosis, however factors that increase the likelihood of the condition are as follows.
 How is it Diagnosed? Unfortunately due to difficult it is to identify many women go undiagnosed for many years with the average being around 7. Currently the only way to confirm a diagnosis of endometriosis is to have a laparoscopy, which is a particular surgery where doctors are able to look for endometriosis tissue within the abdomen and take a sample to examine in a laboratory. During the surgery the grading of endometriosis would be determined as well. Grade 1 (mild): small patches scattered around the pelvis Grade 2/3 (moderate): disease is more widespread and can be found on ovaries and other parts of the pelvis. Grade 4 (severe): Has spread to most of the pelvic organs. If you suspect that yourself or someone else may have endometriosis, please talk to your doctor about any and all symptoms you may be experiencing. A helpful tool has been designed to help health professionals and yourself in identifying and assessing endometriosis symptoms, which may also reach a faster diagnosis. It is called the Raising Awareness Tool for Endometriosis (RATE), which can be accessed through the provided link. RANZCOG - RATE What are your treatment options? Conventional treatment of endometriosis is wide ranging as not all therapies may be effective or the possible side effects could have an overall net negative for a person’s health. It is important to discuss with your doctor about any and all side effects with any treatment options. As stated in the previous blog, currently there is no cure for endometriosis, so in that regard all treatments are aimed at pain management or general management of the condition. Non-manual therapy treatment option
Hormone Therapies, are used to help suppress the growth of the endometrial cells and stop or limit bleeding, including during the menstrual cycle. Examples include:
Surgery: aim is to remove as much visible endometriosis as possible and to repair any damage found.
 Self care treatment It is important to remember that the pain and or discomfort a women may experience from Endometriosis is unique to them and will vary from person to person. With that in mind here are some examples of at home treatments you can use to help with managing your pain. Exercise
Other supportive self care treatments are:
What can my Osteopath do? When treating endometriosis, it is best that a multi-disciplinary approach is used. Where a range of health professionals including your GP work together to provide the best possible care for you. Osteopathy would provide a range of hands on, non-invasive treatment methods to best optimise the body’s natural function. Examples of possible treatments that an Osteopath could provide you are as follows.
 What can my friends and family do to help? The best thing that friends or family can do to help is be a reliable source of support. Many people suffering from endometriosis feel alone in their struggles. Something as simple as bringing your loved one a heat pack when you notice them struggling or allowing them to sleep in a little longer can go a long way in helping someone suffering to feel more validated. Always remember that just because you cannot see the illness does not mean that it does not exist. It is important to remember that symptoms for endometriosis are varied and unique to the individual and that the condition does not have a set rhyme or rhythm. So please be understanding that someone with this condition cannot control or predict when a ‘flare’ will occur. References
How does endometriosis affect fertility? | Tommy's (tommys.org) Where Does Endometriosis Occur | Gynaecology Molloy Endometriosis | healthdirect Endometriosis (who.int) Exploring effect of pain education on chronic pain patients’ expectation of recovery and pain intensity (degruyter.com) Management & treatment of endometriosis | Jean Hailes Treating endometriosis | The Royal Women's Hospital (thewomens.org.au) Endometriosis Australia | Home  By Jamuna Edwards “Sleep is your superpower; it is your life-support system and mother nature’s best effort at immortality. Wonderfully good things can happen when you get sleep, and alarmingly bad things when you don’t, for both your brain and body” (Professor Matthew Walker). The average person will spend approximately one-third of their life asleep, yet it is something not many of us fully understand or appreciate. In this blog, I will cover some of the basics of sleep and give some advice on how you can make it your superpower! Why is sleep so important? An immense cascade of health benefits occur when we sleep. It is often thought that the brain “shuts off”, this could not be more wrong. In fact, your brain is up to 30% more active in certain stages of your sleep cycle. During the day our bodies go through many processes that cause a build-up of waste products and it is during the night, when we are in our deep sleep stages, that these wastes get cleaned away. Sleep is also when we strengthen our immune system by producing antibodies to fight illness, when we undergo tissue repair and growth, and when our minds process our experience of waking life and consolidate all of this into memories. 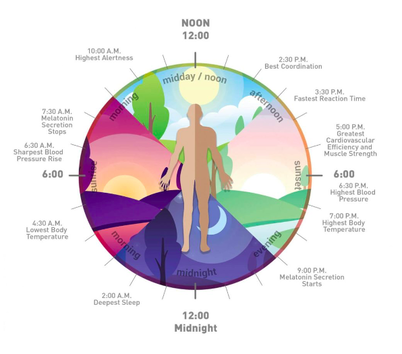 What are the stages of your sleep cycle? We have four stages of sleep, the first three are NREM (Non-Rapid Eye Movement) and the last stage is REM (Rapid Eye Movement) sleep. These stages of sleep alternate throughout the night in a cyclical fashion and different stages affect your brain and body differently! Stage 1: This is the transition from being awake to falling asleep, usually lasting 5-10 minutes. Stage 2: This is light sleep, lasting from between 10-25 minutes. During this stage your heart rate and breathing slows, your muscles relax, eye movements stop, your body temperature drops and brain waves become much slower. Your body is getting ready for deep sleep! Stage 3: Deep sleep, lasting from between 20-40 minutes. This stage is incredibly important for your overall body health, during this stage your body performs maintenance and repair all the way down to a cellular level. Tissues are repaired and regrown, bone and muscle are built, and the immune system is strengthened. This deep sleep is needed for you to feel refreshed and well-rested the next day. Stage 4: Your first REM cycle will occur approximately 90 minutes after you first fall asleep. As the night progresses each REM period will typically get longer, ranging from anywhere between 10 minutes to an hour. During REM sleep, your heart and breath rate increase, your muscles become paralysed (thought to prevent us from acting out our dreams in real life) and brain activity resembles similar levels as when you’re awake. Sometimes the brainwave activity may be even higher, and this is when we have intense and vivid dreams. REM sleep is important because it stimulates areas in your brain that are essential for learning, processing and consolidating your day’s experiences and thoughts to create short- and long-term memories. So, we can see that Stage 3 NREM deep sleep is essential to have a healthy functioning body, just as Stage 4 REM sleep is to have a healthy functioning brain! So that covers the stages of sleep, but what makes us sleepy and what wakes us up? 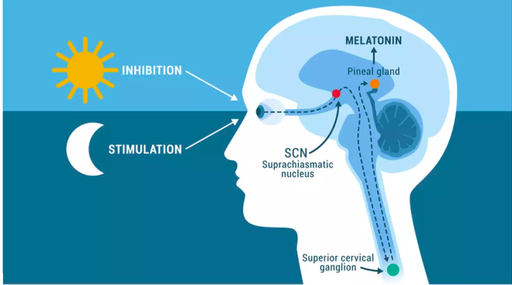 There are two body processes that drive our sleeping and waking periods. They are the circadian rhythm and the homeostatic sleep drive. Circadian rhythms are internally driven 24-hour cycles that are part of your body’s internal clock. Constantly running in the background carrying out many essential functions and playing a vital role in nearly all sys tems of the body. One of its very important roles is the sleep-wake cycle. This rhythm is primarily driven by changes in light and darkness in your surrounding environment. It is regulated by a part of the brain called the suprachiasmatic nucleus. Your brain can tell when the light is changing through the optic nerve in your eyes. As night-time comes and it begins to get dark, the pineal gland starts producing melatonin, while exposure to light prevents melatonin production; thereby synchronising our sleep-wake cycle with night and day. Your exposure to light, especially morning sunlight, strongly reinforces these patterns. Homeostatic sleep drive is the desire for sleep. It grows the longer you stay awake. This desire for sleep occurs because of a build-up of sleep-related hormones in the fluid in the brain and spinal cord, including adenosine, which helps regulate sleep patterns. As these levels increase, the desire for sleep intensifies and your body rams up the response. Then while you are sleeping this build-up of waste products is removed, restoring optimal brain function. How much sleep do we need? According to the National Sleep Foundation Guidelines healthy adults need between 7-9 hours of sleep per night. While babies, young children and teens need more as they undergo more rapid growth and development. These guidelines also recommend that 7-8 hours of sleep is essential for people aged over 65. It is important to remember that 7-9 hours of time sleeping, not just time in bed. So, if you are aiming to only get 7 hours of sleep allow for at least 7.5 hours of time in bed, depending on how easy/difficult you find it to fall asleep.  What happens when we don’t get enough sleep? Sleep is when we restore and repair, how we recover from illness, deal with stressors, consolidate memories and solve problems. While the short-term effects of not having enough sleep is something we have all likely experienced and are very aware of; it is the long-term consequences of sleep deprivation that can wreak havoc on our bodies and brains. A persistent lack of sleep leads to poorer physical and mental health and increases your risk of many health issues including: Cardiovascular disease during deep NREM sleep your heart rate slows, blood pressure drops and breathing rate stabilizes. This reduces the stress on the heart and allows it to recover from the stress placed upon it during waking hours. If you are not getting this restorative sleep your risk of high blood pressure, coronary heart disease, heart attack, and stroke increases. Diabetes sleep deprivation leads to increased levels of cortisol (stress hormone) which results in higher blood sugar levels. In an attempt to balance this out your pancreas will produce more insulin; however, it is not as effective in the presence of cortisol and over time the pancreas cannot keep up with the work of keeping your blood sugar levels normal leading to an increased risk of diabetes. Weight gain and obesity Sleep helps regulate the hunger hormones and not getting enough sleep puts you at a higher risk of overeating and craving higher-calorie dense foods. Hormonal issues Sleep and the circadian rhythms play an important role in regulating many hormones including:
Impaired immune response sleep provides essential support to our immune system. Sleep deprivation has been shown to lead to poorer immune function, including an increased risk of infection in people who sleep less than 6-7 hours. You will also be more likely to catch the common cold or flu. Pain there is a strong relationship between sleep and pain. New evidence shows that the effect of sleep on pain might be even stronger than the effect of pain on sleep. Sleep and pain have a bidirectional relationship, if you are sleep deprived you are at a higher risk of developing pain or that your pain is worsening, while your pain can cause disrupted sleep creating a worsening cycle of sleep and pain. Mental health disorders research has found that brain activity during sleep has a profound effect on our mental and emotional wellbeing. It used to be thought that poor sleep was a symptom of mental health disorders but now the evidence is saying it is mental health disorders that can be a symptom of poor sleep. Both sleep and mental health are very complex issues affected by a multitude of factors, But, considering how closely intertwined the two are, there is reason to believe that getting adequate amounts of sleep can have a very positive effect on your mental health. So now we know how vital sleep is for our overall health, how can we improve it? Prioritize your sleep and have a consistent sleep schedule! We spend so much time planning our waking life, take the time to plan your sleep. Find a night-time routine that works for you
Your daytime activities also affect your sleep quality so here are some more tips on what to do, or what not do for a better night’s sleep
What works for one person won’t necessarily work for another, so it’s worth trying out some different adjustments to find what helps you sleep best. You don’t have to change everything at once, even small changes can make a difference in improving your sleep. It is important to note that changing your sleep habits won’t always resolve sleeping problems and if you suspect you have a sleep disorder then you should consult with your GP to identify the underlying cause and how best to address it. If you want more help figuring out what would work for you any of the team here at HMC can help with lifestyle advice tailored to you and osteopathy can also help by calming the nervous system, decreasing tension in your body and helping to alleviate aches or pains that may be contributing to disrupting your sleep. References Brain basics: Understanding sleep. (2019, August 13). National Institute of Neurological Disorders and Stroke. https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Understanding-Sleep How Much Sleep Do We Really Need? (2021, March 10). Sleep Foundation. https://www.sleepfoundation.org Sleep deprivation. (2021, June 24). Sleep Foundation. https://www.sleepfoundation.org Sleep hygiene. (2020, December 8). Sleep Foundation. https://www.sleepfoundation.org/sleep-hygiene Walker, M. (2017). Sleep the good sleep. New Scientist, 236(3147), 30-33. https://doi.org/10.1016/s0262-4079(17)32022-5 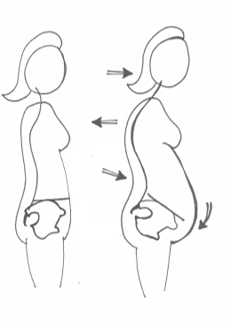 By Ramona Packham Pregnancy demonstrates the body’s incredible ability to adapt to change, nurture growth and produce life. As a baby grows, the mother’s body changes to create more space. Organs get squashed, the diaphragm moves up, the rib cage widens, the muscles of the back work overtime to compensate for the muscles at the front being stretched, the curves in the spine increase, and the pelvic floor takes on an increasing amount of downwards pressure. Given all these wonderful changes, it is not surprising that some pregnant and post-partum women experience conditions that can cause discomfort, pain, stress, and anxiety. Incontinence, separation of the abdominal muscles, and scarring are three of these conditions, and there are strategies available to assist in recovery. The Pelvic Floor Let’s revise an important structure relevant to these conditions, the pelvic floor. Have you ever been told to strengthen your ‘core’ muscles? A lot of people perceive this as the six-pack muscle between the ribs and pelvis. While this muscle forms part of the core, it is just one piece in the puzzle. Think about your core as a cylinder. The broad diaphragm muscle that allows us to breathe forms the roof, and the pelvic floor forms the floor, hence its name! The pelvic floor supports the bladder, uterus, and bowel, and facilitates the birthing process. As a baby grows, the downwards pressure on the pelvic floor increases. The pelvic floor also works to maintain continence, and functions hand in hand with the abdominal muscles. In the pregnancy and post-partum population, the pelvic floor creates a passageway for the baby to move through in birth and helps to maintain continence afterwards. Incontinence Approximately 33% of women experience bladder or bowel incontinence after giving birth. While this is an outcome for some pregnant women, it is not inevitable, and it is recoverable. If you suffer from incontinence, seek help. The health of the pelvic floor affects both bladder and bowel continence. The pelvic floor can be weak and underactive or tight and overactive and both can lead to incontinence and produce similar symptoms. If you have a weakened or underactive pelvic floor, symptoms include the feeling that you just can’t hold on when needing to go to the toilet, or accidentally losing control over your bladder or bowel. On the other hand, if your pelvic floor is tight or overactive, you might experience painful sexual intercourse, pelvic pain, straining when going to the toilet, constipation or a feeling of incomplete emptying, or stress incontinence when participating in certain types of exercise, coughing, sneezing, or laughing, It is important to find out the type of incontinence and the reason for it as this will be a guide to the most effective management. Many women recover from incontinence following pregnancy without doing anything specific, as the tone of the pelvic floor often improves by itself over time. However, there can be residual weakness and recovery can be enhanced with the implementation of simple, time-effective techniques, including pelvic floor and postural work. Postural changes can reduce leaking in women with stress incontinence. Some postural elements a health professional will assess include:
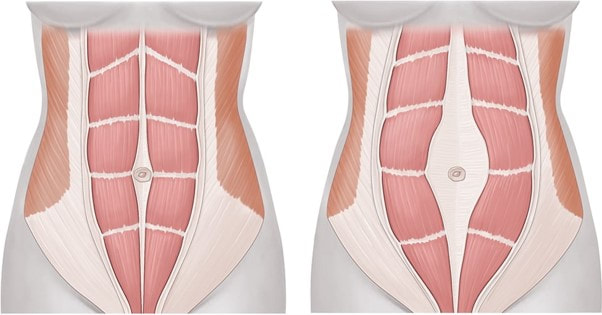 Diastasis Recti A diastais recti (DR) is a separation of the large ‘six-pack’ muscle in the abdomen where it joins in the middle of the trunk at a line called the linea alba, a sheet of connective tissue between the muscles. A DR can also be linked to weak pelvic floor muscles. Some separation is normal in pregnancy, and it occurs as the uterus grows and the abdominal muscles stretch. 100% of women have some diastasis at their due date, but most resolve within 6 weeks post-partum. 39% will still have some diastasis 6 months post-partum, and these women are more likely to have urinary incontinence. A DR does not need to be a lifelong condition, they can resolve with time and management. The linea alba requires some training to repair, just like muscles need to be strengthened after injury. The aim is to activate the deep abdominal muscles and pelvic floor, and then to improve the relationship between these groups. This can be achieved through practicing specific exercises. When completing any exercise with a DR, it is important to monitor for bulging in the space of the DR as this indicates that the muscles may not be contracting as well as they could be. Practice: Observe how flat your abdominal muscles are. Tense your abdominals using your hands to feel what is happening. When you contract, your abdominals should stay nice and flat, and there should not be any bulging outwards. It is likely that during pregnancy you will need to reduce the amount of exercise, or the load used during exercise, to regulate the pressure going through your abdominal wall. It is especially important for women who have been pregnant in the past to reduce the amount or load of activity earlier on in their pregnancy as the linea alba has been stretched before and will fatigue faster compared to women who are pregnant for the first time. Continue exercise and abdominal work, but do not challenge the body to extremes. Recovery is a marathon, not a sprint! Get help from a pelvic health professional Pelvic health specialists strongly recommend women to have their pelvic floor assessed and rehabilitated following childbirth. Professionals like osteopaths, women’s health physiotherapists, pelvic health physiotherapists and clinical Pilates instructors can complete these assessments and prescribe a range of specific exercises and therapeutic techniques to suit your body in its recovery. They also assess the position and movement of your rib cage, spine and pelvis which work together to facilitate optimal contraction of muscle. Seeking help from these professionals will facilitate your body’s natural healing, prepare for optimal results from exercises, and provide relief from pain and discomfort. Further recommendations on managing incontinence and DR include:
C-section scars and stretch marks: may contribute to mild pelvic discomfort In Australia, approximately 36% of women giving birth deliver through caesarean section (C-section). Before we discuss the residual scarring following a C-section, let’s talk about fascia. Fascia is often described as the glad wrap of the body, as it forms a covering over our muscles and creates a smooth pathway for vessels to travel through. Fascia is an important structure in the abdomen, where it holds organs in place and allows them to move freely. When we have scars anywhere in our abdomen, pelvis or even our back, the fascia can become tight and pull organs in different directions making them less movable. This may be interpreted in the body as pain, restricted movement, and a reduction in overall function. Thankfully, the body possesses extraordinary self-healing properties that can work to reduce fascial pulling that occurs with scarring, and aid recovery. Osteopaths use hands on therapy to treat scarring from C-sections and other surgical procedures frequently. One of the best things about scar tissue recovery is that some techniques can be done by yourself. Anytime. Anywhere. If you live with family or friends, you can even teach them to apply these techniques for you (less work for you, more fun for them). Scar tissue massage is easy to learn and may deliver great results with a little bit of commitment. Here are three ways you can begin your scar tissue massage:
Exercise during pregnancy Physical and mental health are key to a positive pregnancy and post-partum experience. Participating in regular, moderate intensity exercise is recommended during all stages of pregnancy for reasons which include:
 Mind health The emotions tied to pregnancy and post-partum recovery can be overwhelming and difficult to manage. Connecting with people you trust is a great way to build a supportive network. One in five expectant women and one in ten expectant men experience anxiety and/or depression during pregnancy and in the first years of parenthood, which is why organisations like Perinatal Anxiety and Depression Australia (PANDA) have been established. PANDA offers Australians a National Helpline and other resources that can be found on their website to aid recovery. Their helpline is available on 1300 726 306 Monday-Friday, 9am-7:30pm (AEST). The PANDA website may be accessed through this link PANDA - Perinatal Anxiety & Depression Australia Other local businesses that may be helpful during the pregnancy and post-partum period: Secrets from the Honey Tree Secrets from the Honey Tree – Eumundi Traditional Health and Healing Centre located in Eumundi Pelvic health Physiotherapist, such as Pre and Postnatal Care (alchemyinmotion.com.au) located in Noosa By Kirby Edwards Hi HMC team! Recently I have been having a few discussions about anxiety and stress. So, I thought I would share some of my tools that I have in my tool kit. Please note, I am not a psychologist, doctor, counsellor, or psychiatrist. This is my ever-growing tool kit (and am open to more suggestions, the more tools the better!) If you feel like you need a little extra help, there are resources available including counsellors, psychologist, psychiatrists, lifeline, beyond blue and your GP. Your GP is the best avenue to pursue counsellors, psychologists and psychiatrists. And Lifeline and Beyond Blue are fully staffed with 24-hour hotlines So what is Anxiety..? Anxiety is our body’s way to alert us to danger. Short term it is a good thing because the body releases hormones that stimulate our sympathetic nervous system (fight or flight) and helps us to react to fearful or stressful situations quickly. Short term this is amazing! Long term, it is not ideal. Anxiety is a unique experience and can feel different for everyone. Some people may not have ever experienced it and some people may experience it but not know what it is. Be kind, you never know what someone is going through on the inside. While there are different types of anxiety and it is very individual, beyond blue talks about some common signs and symptoms including:
Here are some tools that may help you if you are experiencing any of the symptoms of anxiety: Breathe Breathing is your best friend, and a necessity. We know that our body is so clever that we can breathe without thinking, but when was the last time you took a conscious breath? Sometimes we forget to breathe or might find yourself even holding it. Let it go… a nice slow exhale. A deep breathe in and doubling your exhale stimulates your vagus nerve, which is a branch of your parasympathetic nervous system also known as our ‘rest and digest’ state. This will help to steer you away from the elevated ‘fight or flight’ mode (the sympathetic nervous system) that we are in when we are stressed/anxious. Check out other HMC blogs for more information on the benefits of breathing. There is also a great book called “Breathe” by James Nestor that has lots of great info. 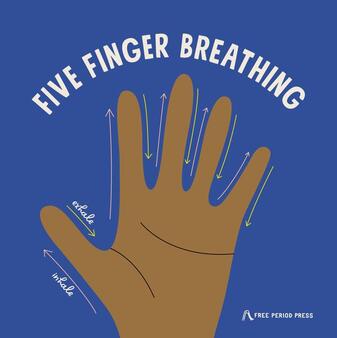 Hand/finger Breathing A great one for kids and adults alike. Hold up one hand in, stretching the fingers out. We are going to trace our fingers with our other pointer finger. Start at the thumb and trace it slowly from the bottom to the top of the thumb as you BREATHE IN, when you get to the top, trace the thumb slow down as you BREATHE OUT. Repeat this all the way along the fingers – repeat on the other hand if you need to. Journaling Either writing or use your voice memos on your phone. Sometimes we just need to get our thoughts out of our head to remind us you are not your thoughts, it is feelings, and what you feel is valid, but feelings will pass. Feel Good List When you are feeling good, write down a list of things that you enjoy or that make you feel good, then when you’re not feeling great you can look at the list and pick something… For some of us at HMC it’s nature, surfing, yoga, breathing, nature, music, swimming or hugging our kids/grandkids or a tree…  Move Movement or exercise can help you get out of your head… it releases good endorphins which can help shift your mood. The benefits of exercise/movement are epic. I say move because it doesn’t matter what you do, just start. Research has shown 10 minutes a day is helpful to shift your mood. That’s 3 songs if you like dancing, about 1 kilometre of walking, sweeping and mopping the floor (or half of it if you have big house), parking a bit further away to walk to the shops. Get creative but get moving. Try it! Sometimes I like to walk and talk into my voice memos, there is a feeling of moving forward from whatever is going on at that time for me. Sleep Taking care of your physical health supports your mental health as well. Due to the many aspects of sleep and anxiety, getting better sleep may help combat feelings of anxiety. Examples of possible changes include, building healthier sleep habits/hygiene, limiting stimulants such as caffeine and alcohol, relaxation techniques or breathing. Previous blogs on our HMC site include information the importance of sleep and sleep hygiene/routine and boosting our immune systems. The implementation of these small but powerful habits can have a big impact on how your body/mind responds to stressful situations. Diet Research has been shown that a healthy diet can assist with anxiety. A poor diet, which consists of foods with high sugar, salt and fat content, highly processed and low nutritional value, could lead to an increased risk of experiencing anxiety (amongst other things). Eating a balanced diet including fresh fruit, vegetables, whole grains, limited fat dairy, lean poultry and meant, legumes, seafood, nuts and delicious healthy oils can help to minimise anxiety.  Alcohol and Caffeine These guys get their own tab. Alcohol is a depressant and caffeine has a half-life of 3-7 hours and as a result may make it difficult to sleep if consumed too late. I generally cannot have full caffeinated coffee after 11.30am to 12 noon. Due to the characteristics of alcohol and caffeine, they can aggravate anxiety or trigger panic attacks in certain people. Limit the intake, switch to decaf or try some alcohol-free or low alcohol options as an alternative.  Self-talk or Observing your Thoughts Negative self-talk can be a challenging cycle to break or shift to a more positive self-talk. One way to do it is to think of what you might say to a child or to a dear friend that is having a hard time. Also, a reframing of the language can help to shift your perspective to understand that is not going to be forever. For example, instead of “I have anxiety, it’s just the way it is” we could try “I am experiencing some anxiety at the moment, it will pass. I will breathe and look for some tools to manage it.” Or instead of “I should not feel like this” try “I am learning how to manage this”. If this is interesting to you, it might be worth looking for a counsellor/psychologist etc, that works with Cognitive behavioural therapy (CBT) or Acceptance and Commitment therapy (ACT). By observing your thoughts, you can start to correlate triggers or patterns. This can be helpful to mitigate anxiety. For example, if I know I have a stressful situation coming up, I exercise beforehand. Over the years of trial and error, I have found that by exercising beforehand, I have a better handle on the situation, and I am more likely to respond, rather than react. Another question to ask yourself is “is it mine?”. We can sometimes find ourselves getting caught up in other people’s emotions/stresses etc. This is a very compassionate and empathetic way to be, however, is it really necessary to carry other people’s anxiety/stress around as well? This self-questioning is NOT a blame game, this is just a reminder to take a moment, a deep breathe and ask if this emotion is yours, if it is not than it is ok to let it go. If it is yours, then breathe again. Supplements that can support Some handy ones I keep in my handbag include - Emergency Bushflower essence, bach flower or rescue remedy drops, ashwagandha tablets, lavender oil. You should always speak to your doctor or health professional before starting on supplements as they may interact with certain medications and may be toxic to the body in large quantities and/or may not be suitable for you for various reasons.  Take some time for you You cannot pour from an empty cup, so what fills up your cup? Is it the soul nourishing humans you need to make a call to or is it that walk around the block that you missed to keep you grounded. Refer to your list of “feel goods” if you need to. Communicate with your family, friends, and your Team Reach out if you need to, chances are you know someone else who has also experienced anxiety to some level. One of the phrases I use is “Hi friend. I am currently experiencing some anxiety, could you please listen to me, I do/don’t need someone to solve my problem right now, I need someone to listen.” This statement may rustle a few feathers at first but the direct way of communicating means that person is aware of what you need right now in your current situation. There is no guessing. Not everyone has experienced anxiety and as it is such a unique experience, some people don’t know how to help when you reach out. If you are reaching out to them, it is likely they love you and will want to help. Try not to be shy about what you need at that time. Counting Sometimes counting can be helpful. Counting to 10 while taking some deep breathes can sometimes be a quick change from reactive to responsive.  Gratitude Benefits of gratitude include enhancing mood, positive emotions and thoughts, better communication, improved physical health (including sleep) and more! This research has found that our brain releases dopamine and serotonin, which are two feel ‘good’ neurotransmitters when we express gratitude. In some studies, it has also shown to reduce pain and release toxic emotions. Sometimes I forget this, so for me to be accountable, I recruit a friend, at the end of each day we text each other 3 things we are grateful for… Eg. “Hi friend, today I am grateful for fresh water, friends and my dog”. I have some friends that do it with their children at the end of the day. Meditation Even just 5 minutes a day can make a difference – take that 5 minute of your screen/scrolling time and meditate instead… My favourite is ‘yoga nidra’ on you tube. A previous HMC blog is about Progressive Muscle Relaxation, which is also a goodie! 3-3-3 rule Look around you and name three things you can see, three things you can hear, three things you can feel. Also do a quick body scan and unclench anything that is clenched. Some common ones are your shoulders, jaw, pelvic floor or hands… Stay hydrated! If we are not hydrated enough, it can lead to restlessness, poor concentration, low energy and agitation.  Superman Power Pose Ok, this one is a bit far out but try it, do it on your own if you like but this pose – standing with your feet hip distance apart, hands on hips, chest out and eyes forward or slightly looking up – can help shift your mood. Podcasts There are a lot of good podcasts out there, take it all with a grain of salt and trial a few to see if they help. Some of my favs include the Huberman Lab, the Mindset Mentor, Ted talks, anything by Brene Brown, oh also sometimes you just need to laugh – so throw a funny one on and laugh until you feel lighter! How can osteopathy help? The mind-body connection is undeniable. Even for people who don’t experience anxiety, even just listen to your body when you are nervous about something or excited? Butterflies? Sweaty palms? Increase in heart rate? That’s your body responding to your mind. Some of the principles of osteopathy include:
With regards to anxiety, Osteopathy can help with working on:
Some previous blogs have some information that may be helpful including a progressive muscle relaxation, breathing, sleep and the lymphatic system… oh who am I kidding, they are all GREAT reads ☺ Remember you are worthy, you are not your thoughts and it will pass. You can only control what you can control, try not to spend too much (if any) time in the what ifs, and more time in gratitude. You don’t have to stay in this state of anxiety, it is often treatable. It is just a matter of exploring the best fit for you. Some of these lifestyle changes listed here may be enough to help. Or you may need to seek more help from the below resources or your GP or a counsellor. There is help available. Take care and be kind to yourself (and each other). Cheers Kirby ☺ Resources https://www.blackdoginstitute.org.au/resources-support/anxiety/ https://www.beyondblue.org.au/the-facts/anxiety/signs-and-symptoms https://www.lifeline.org.au/get-help/information-and-support/anxiety/ References and further resources below: https://www.hmcosteopaths.com/blogs http://www.thecalmcorner.com/2018/11/material-share-monday-5-finger-breathing.html https://positivepsychology.com/neuroscience-of-gratitude/ https://www.facebook.com/totalbalancehealth/photos/happiness-chemicalsim-sure-you-have-heard-about-all-these-different-chemical-com/3301269156585465/ https://dietitiansaustralia.org.au/wp-content/uploads/2016/07/NR06_pg014-anxiety-Tania-Matthewson.pdf https://www.sarahwilson.com/2017/01/interrupt-anxiety-with-gratitude/ https://www.sleepfoundation.org/mental-health/anxiety-and-sleep https://blog.ted.com/10-examples-of-how-power-posing-can-work-to-boost-your-confidence/ By Angus Nichol Over the past couple of years, it has been impossible to escape the all-encompassing pandemic we’re currently living through. There has been a lot of emphasis placed in the media about the importance of vaccination to protect us against coronavirus, but there has been limited information given about how we can support our body’s immune system to give us the best chance of fighting it off… well, any type of infection. This may be particularly important as restrictions start easing and the promise of national and international travel (for people and the viruses they carry) becomes more realistic. The lymphatic system can be thought of as the body’s “sewerage system”, and it plays an important role in enhancing and facilitating the function of the immune system, as well as other important roles in maintaining fluid balance and aiding the absorption of dietary fats for metabolism and storage. However, this blog will focus on the lymphatics system role in immunity, how osteopaths and other health professionals can support your lymphatic and immune health, and other ways that you can keep your lymphatic (and immune) system strong enough to fight off whatever potential invaders life throws at us! So… what is the lymphatic system? The lymphatic system is a division of the body’s circulatory system that is separate, but also closely related to the vascular system. It consists of a network of lymphatic vessels and nodes, as well as various organs that have specialised functions. The lymphatic system helps protect the body against infection by producing white blood cells called lymphocytes, which help the body fight off disease-causing microorganisms. The organs and tissues of the lymphatic system serve as major sites of production, differentiation, and proliferation of two types of lymphocytes—the T lymphocytes and B lymphocytes (aka T and B cells). Although lymphocytes are distributed throughout the body, it is within the lymphatic system that they are most likely to encounter foreign microorganisms. Here are some of the major components: 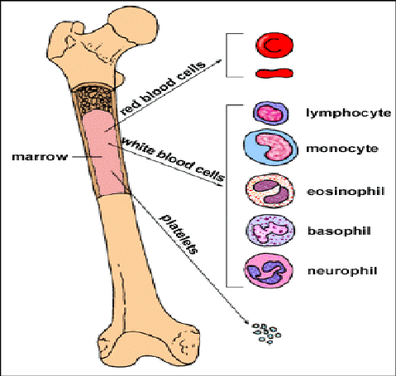 Bone marrow - The bone marrow it’s the soft, squishy substance inside the hard outer casing of the bone. All lymphocytes derive from stem cells in the bone marrow. Stem cells destined to become B lymphocytes remain in the bone marrow as they mature, while prospective T cells migrate to the thymus to undergo further growth. 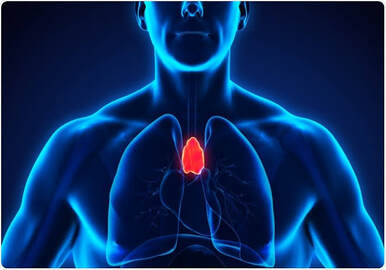 Thymus - Your thymus sits in the upper part of your chest ,just behind your sternum and in front of the heart. This is where T lymphocytes (T cells) proliferate, differentiate and mature. 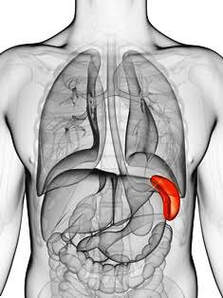 Spleen - The spleen sits behind your lower ribs on the left side. One of it’s main functions is that it acts as an interface between the vascular and lymphatic system, bringing blood into contact with lymphocytes. Both blood and lymph (lymphatic fluid) contain specialised cells that aim to identify, destroy and remove disease-causing microorganisms. 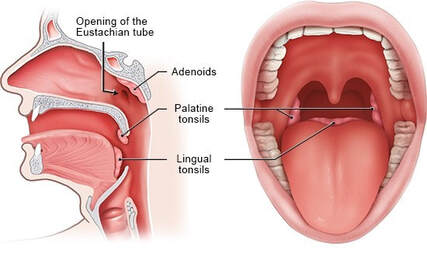 Tonsils - Humans have three sets of tonsils. The tonsils at the back of our throat that we think of are known as palatine tonsils, however we also have adenoids and lingual tonsils. These act as security guards to ward off any nasty foreign intruders trying to enter the body through the mouth and nose. They also contain B and T cells used to fight infection. 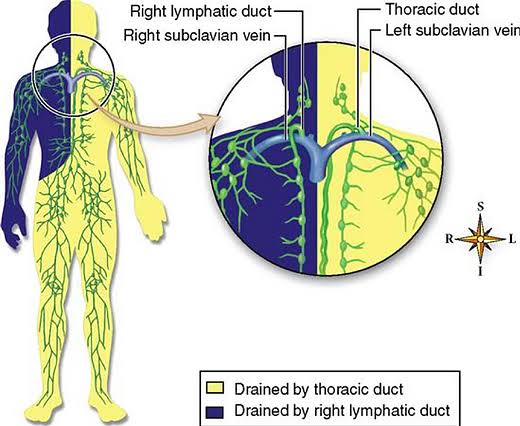 Lymph nodes - The lymph nodes, or lymph glands, are small, encapsulated bean-shaped structures composed of lymphatic tissue. Thousands of lymph nodes are found throughout the body along the lymphatic routes, and they are especially prevalent in areas around the armpits (axillary nodes), groin (inguinal nodes), neck (cervical nodes), and knees (popliteal nodes). Lymphatic vessels - The lymphatic vessels connect all the lymphatic organs to form the plumbing or sewerage network in your body. They transport fluid away from tissues and are similar to blood vessels, but they don't carry blood. The fluid transported by lymphatic vessels is called lymph. Lymph is a clear fluid that comes from blood plasma that exits blood vessels at capillary beds.This fluid becomes the interstitial fluid that surrounds cells. Lymph vessels collect and filter this fluid before directing it toward blood vessels near the heart. It is here that lymph re-enters blood circulation. Lymphatic vessels from various regions of the body merge to form larger vessels called lymphatic trunks. The major lymphatic trunks are the jugular, subclavian, bronchomediastinal, lumbar, and intestinal trunks. Each trunk is named for the region in which they drain lymph. Lymphatic trunks merge to form two larger lymphatic ducts.  How can your Osteopath help? So, now we know what the lymphatic system is and how it works… but how can your local osteopath treat the lymphatic system, and aid your immune system? I’m glad you asked. Two of the main principles of osteopathy is that structure governs function, and that the body works as a unit. Lymphatic vessels may be squished by overlying musculoskeletal structures such as tight muscles and fascia (connective tissue), much like standing on or running over a garden hose. Furthermore, stiff joints may may cause kinks in these internal hoses and reduce our mobility, thus restricting the flow of lymph through our sewerage system. Osteopaths can assess where there might be be lymphatic blockages present. We can then use a variety of soft tissue/massage, joint articulation and other movement based techniques to relieve the pressure on lymphatic vessels and clear the blockages in our plumbing system. This will encourage the free flow of lymphatic fluid, thus increasing the circulation of all those disease-fighting cells around the body. Furthermore, osteopaths may also manipulate the connective tissues surrounding organs (for example, the spleen or tonsils) to encourage optimal function of these organs. Pretty cool, huh? But guess what… there’s plenty of other health professionals who can help in treating the lymphatic and immune systems. GPs are the gatekeepers of serious disease, and they may prescribe you with medications or send you off to a specialist specific to your immune condition. Naturopaths, Traditional Chinese Medicine (TCM), Acupuncture and Kinesiologists can be invaluable alternative therapies that may help you to assess vitamin/nutrient deficiencies and prescribe natural alternatives to pharmaceuticals and/or supplements to help boost your immune system for prevention and treatment of immune conditions. Even though there are plenty of professionals out there who can help, in the end it’s YOUR body and YOUR immune system… and guess what, there are some simple and effective ways to optimise your own immune and lymphatic health. Vaccination isn’t the only way to fight disease. Let's start with the simple things that you may already be practicing in your everyday routine...
This seems like a lot, but each thing you do has an additive effect in enhancing your immune system health and overall wellbeing. So, start with something small and try to make it a habit, and then add more good habits over time!  Do you want to know a few more specific ways to promote your lymphatic function…? I got you! Swimming, yoga, dancing and trampoline all use gentle (and sometimes less gentle) full body movements that can help release tension in your muscles and fascia, improve joint mobility and encourage lymphatic flow through your body. Furthermore, regular breathwork (see my previous breathwork blog for beginners) can help the body’s primary pump (well… maybe after the heart) to get you up and moving. Furthermore, there are a wide variety of supplements that are available to help support the immune system. You should always speak to your doctor or health professional before starting on supplements as they may interact with certain medications, can be toxic to the body in large quantities and/or may not be suitable for you for various reasons. Here, I will focus on three supplements which may help support the body’s immune response to coronavirus. Vitamin C - An antioxidant and free radical scavenger that has anti-inflammatory properties, helps strengthen blood vessels and influences cellular immunity that may help to protect against infection. Good dietary sources of Vit C include broccoli, capsicum, potatoes, tomatoes, citrus fruits and many more! Vitamin D - Vitamin D has been theorised to be a protective against coronavirus. One study found that regular Vit D supplementation was associated with 34% less chance of COVID-19 infection. Sun exposure helps your body to naturally create Vitamin D, so spend a bit of time (but not too much) soaking up some rays. Zinc - Zinc may help prevent COVID-19 from entering the body through three complex mechanisms; it may also directly prevent the ability of the virus to replicate; and also helps to balance out the immune system’s reaction to coronavirus. So, whether you’re trying to avoid COVID-19 infection, trying to prevent side-effects after vaccination or boosters, or just want to support you general well-being… visit your local osteopath or other healthcare practitioner and ask how they can help you to support your own immune and lymphatic systems! Stay healthy and stay happy!  By Sam Dyer Do you suffer from foot/heel pain...? Could it be Plantar Fascitis? Firstly, what is Plantar Fascia? Plantar fascia is connective tissue that starts from the middle of your heel and inserts into the different tendons of all five toes. It is a really important structure to ensure that you are using your foot correctly, it has crucial role in keeping the foot stable during all types of movement and plays a role as shock absorber. The plantar fascia, for many reasons, can become damaged. Most commonly by repetitive stress (micro trauma) when this happens the plantar fascia becomes strained/ stretched or inflamed it is labelled plantar fasciitis. It is one of the most common causes of heel pain!! How do you know if you’re suffering from plantar fasciitis? There are numbers of ways that it may present, so if you are suffering from heel pain, I’d recommend coming in and seeing one of our osteopaths to help you get to the bottom of your pain, but, there are a couple of things that you can look out for that might point you in the right direction.
What can you do at home to help relieve some of your pain? Whilst there are some practical things you can be doing at home to assist with your plantar fasciitis, for long term recovery it is important to get to the bottom why the plantar fasciitis occurred in the first place. As I mentioned in the previous paragraph that’s were our osteopaths can be super beneficial in helping assist with your diagnosis. However here are a few things that may assist in pain reduction and can be great place to start!
If any of these causes more pain then its best to cease immediately and seek some further advice/ treatment. If you have been struggling with any of the above symptoms for more than a week or two it’s time to get some extra assistance. That’s where any of the osteo’s at HMC can HELP YOU, osteopathic treatment can be extremely effective in assisting anyone suffering plantar-fasciitis. 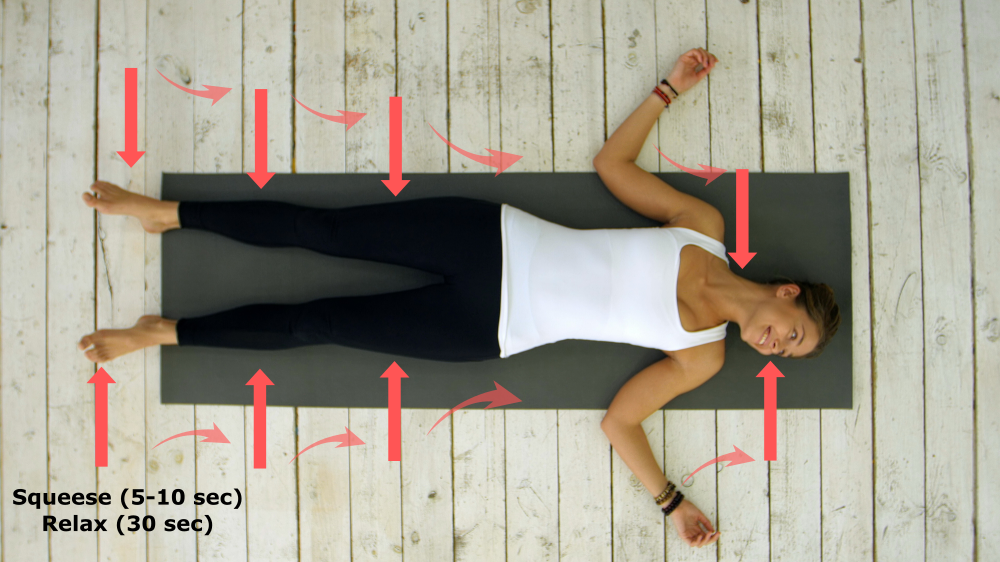 In our everyday life it is unavoidable that we will experience a certain amount of stress. However, although some stress is a normal part of life, it is important to recognise when it becomes excessive and to understand that it can contribute to exacerbating your pain levels, chronic disease and mental health issues. Stress, anxiety and fear cause a multitude of effects throughout the body including muscle tension. This is part of a process that helps our bodies prepare for potentially dangerous situations putting us in a “fight or flight” mode even though some of those situations may not actually be dangerous, our bodies will still respond in the same way. Sometimes we don’t even notice how our muscles become tense, or that we are clenching our jaw often resulting in tension headaches and even contributing to back pain. A technique that has been widely used and recognised as being effective in reducing muscle tension is Progressive Muscle Relaxation (PMR) in which you tense up and relax different muscle groups, one at a time, starting at the toes and working up to the head. This will help you recognise where you have tension in your body and help you to release it. PMR can have many benefits, including:
Preparing for PMR - When first beginning consider the following:
During this exercise, each muscle should be tensed, but not to the point of pain or discomfort. If you have any injuries or pain, you can skip the affected areas. Notice the feeling of releasing tension in each muscle and the resulting feeling of relaxation. Let's begin! Sit back or lie down in a comfortable position. Shut your eyes if you’re comfortable doing so. Begin by taking a slow deep breath and noticing the feeling of air filling your lungs. Hold your breath momentarily and then release the breath slowly visualizing the tension leaving your body. Now, move your attention to your feet. Begin to tense your feet by curling your toes and the arch of your foot. Hold onto the tension and notice what it feels like. (Hold for 5 seconds) Now release the tension in your feet. Notice the new feeling of relaxation. Next, begin to focus on your lower legs. Tense the muscles in your calves by pulling your toes towards your head. Hold them tightly and pay attention to the feeling of tension. (Hold for 5 seconds) Now release the tension from your lower legs. Again, notice the feeling of relaxation. Remember to continue taking deep breaths. Next, tense the muscles of your upper leg and pelvis. You can do this by tightly squeezing your thighs and knees together. (Hold for 5 seconds) And release. Feel the tension leave your muscles. Now begin to tense your stomach and chest. You can do this by sucking your stomach in. Squeeze harder and hold the tension. (Hold for 5 seconds) Release the tension and allow your body to go limp. Let yourself notice the feeling of relaxation. Continue taking deep breaths. Breathe in slowly, noticing the air fill your lungs, and hold it in briefly then release the air slowly. Feel it leaving your lungs. Next, tense the muscles in your back by bringing your shoulder blades together behind you. Hold them tightly. Tense them as hard as you can without straining and keep holding. (Hold for 5 seconds) Now release the tension from your back. Feel the tension slowly leaving your body, and the new feeling of relaxation. Notice how different your body feels when you allow it to relax. Next tense your arms all the way from your hands to your shoulders. Make a fist and squeeze all the way up your arm. (Hold for 5 seconds) Release the tension from your arms and shoulders. Notice the feeling of relaxation in your fingers, hands, arms, and shoulders. Notice how your arms feel at ease. Move up to your neck and your head. Tense your face and your neck by tensing the muscles around your eyes and mouth. (Hold for 5 seconds) Release the tension. Again, notice the new feeling of relaxation. Finally, tense your entire body. Tense your feet, legs, stomach, chest, arms, head, and neck. Tense harder, without straining. (Hold for 5 seconds) Now release. Allow your whole body to go limp. Pay attention to the feeling of relaxation, and how different it is from the feeling of tension. Begin to wake your body up by slowly moving your muscles. Adjust your arms and legs. Stretch your muscles and open your eyes when you’re ready. Practice means progress. Only through practice can you become more aware of your muscles, how they respond with tension, and how you can relax them. Training your body to respond differently to stress is like any training – practicing consistently is the key. To begin with, listening to a guided recording may be helpful until you get the hang it of it. Otherwise you could always use mobile apps like headspace or wellness and meditation podcasts. Here is a YouTube link to a Johns Hopkins guided video on PMR. https://www.youtube.com/watch?v=ClqPtWzozXs If you need more help managing stress and muscle tension the team at HMC osteopaths can help with both manual therapy and lifestyle advice tailored to your specific needs. By Angus Nichol Breathing is one of the most basic, yet fundamental, processes necessary for all of life – and it can have a significant impact on our mental and physical wellbeing. Each and every breath influences the activity of every cell in your body - fuelling the burning of oxygen and glucose to produce energy. This energy is used for muscular contraction, organ function and glandular secretion, mental processing, and many more important functions. Normally, adult humans breathe 12-20x per minute – that’s between 17,300 and 28,800 breaths per day. However… what if I told you that YOU’RE DOING IT ALL WRONG?! (Don’t worry, most of us are). How do we breathe? Before we can try to understand the benefits of breathing, we should learn a bit more about how breathing occurs… Breathing is an automatic process that is largely regulated in the primitive part of the human brain (the “brainstem”). Because it occurs automatically, we often take our breathing for granted and do not direct conscious awareness to it, unless it becomes abnormal. When we breathe in (inspiration), our diaphragm (main breathing muscle) contracts and lowers down towards our abdomen and the muscles between our ribs help to expand the chest wall, these processes allow our lungs to expand and fill with air (and most importantly, oxygen!) within the chest cavity. Breathing in through the nose is preferable to open-mouth breathing, as our nose is designed to filter and clean the air before it enters the lungs. When we breathe through our mouth, there is no filtration process and more nasty little bugs and pollutants from our environment enter our body, which increases the risk of chronic health conditions. Conversely, when we breathe out (expiration), the diaphragm relaxes and moves back upwards towards the chest cavity, the chest wall condenses, the lungs deflate and air (carrying carbon dioxide and other waste products from the body) is forcefully ejected out. Breathing – How does it affect our mind and body? Have you noticed that your breath changes depending on your thoughts and feelings? Our mind and bodies share an intimate link, and our mental state has a large impact on our physical state. Different emotions cause us to perform different expressions and gestures. For example, when we’re happy, we smile; when we’re sad, we frown. A similar relationship is present with breathing. When we feel calm and safe, we breathe more deeply and slowly; whereas when we are stressed, our breathing may become shallower and faster. This is because we are under control of our Autonomic Nervous System (ANS). This nervous has two divisions: Our Sympathetic Nervous System (SNS) – This is responsible for our “fight or flight” response, and causes our heart rate to increase, dilates our pupils, stimulates the release of stress hormones such as adrenaline which makes us sweat and feel agitated, and cause our muscles to become tense. It also makes our breathing shorter and sharper. Extended activation of our SNS means that our heart is working overtime, and the prolonged release of stress hormones can have damaging consequences on our bodies that lead to chronic diseases such as heart, stroke and vascular disease, and mental health disorders. This system also plays a role in sensitizing nerves that supply our bones and muscles and make us feel pain. This may cause us to feel more pain than we should for a given injury, or experience pain for longer than we would normally expect (which may be why you come to seek our care!). Our Parasympathetic Nervous System (PSNS) – This may also be referred to as our “Rest and Digest” system, and helps to create a relaxing effect on the body by slowing the heart rate, stimulating digestion, and slowing our breathing. It also has a calming affect on our minds. When we are in “rest and digest” mode, we give our bodies a chance to recover and heal, and become more balanced. So, to put it simply, by consciously paying attention to our breathing and working to breathe slowly and deeply, we can suppress our SNS (fight or flight) system, and activate our PSNS (rest and digest) system – thus making us feel more calm and relaxed. Long term, it may also mean that we can decrease our risk of many types of mental and physical chronic diseases, and may also help decrease the amount of pain we feel in chronic pain conditions. Controlling your breath Great, now we know how breathing occurs, and why breathing properly is important for our health. So, where do we start?! Yogis knew that controlling your breath was important long before it was researched in modern medicine, and they developed techniques to control the breath, which is known as pranayama (coming from the root words prana = ‘vital energy’, or ‘life force’; and yama = ‘control’). Basically, pranayama techniques use breathing to influence the flow of energy within the body. There are many different types of breathing techniques, each with their own benefits, but let’s start with basics: Natural breathing 1. Sit in a comfortable, upright posture or lie on your back, and relax the whole body 2. Observe the natural and spontaneous breathing process (but breathe through your nose!), developing awareness of the rhythmic flow of breath. Do not try to control the breath in any way. You can shift your awareness to the following areas:
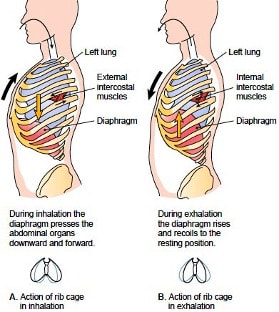
Try to take notice of your breathing rhythm. How fast or slow is it? How shallow or deep is it? Also take notice of how you are feeling, and see if you notice that your emotions are affecting your breath. Abdominal (diaphragmatic) breathing 1. Lie on your back and relax the entire body 2. Place your right hand just above your belly button, and your left hand over the centre of your chest 3. Inhaling through the nose, “Breathe into your stomach” and focus your attention on your right hand moving up towards the ceiling (or stars) with inhalation, and down with exhalation.
compressing back towards your spine until there is no air left. Many of us do not use our diaphragm to its full potential when we breathe. This technique teaches us to activate it more completely and improve our capacity to take air into the lungs. Rhythmic breathing (box breathing) 1. Lie in a comfortable, upright posture or on your back, and relax the entire body 2. Take a few moments to observe your natural breathing rhythm 3. Inhale slowly and deeply through the nose, allowing the abdomen to expand fully (try to breathe so slowly that little to no sound of the breath can be heard) – try to make this inhalation last 4 seconds. 4. At the top of the inhalation, hold your breath and mentally count “1,2,3,4”, before slowly exhaling (through the nose), feeling the abdomen be drawn back towards the spine. Also try to make this exhalation last 4 seconds. 5. At the end of the expiration, mentally count “1,2,3,4” before starting the next inspiration.
Consciously slowing our breathing will help dull down the SNS ("fight or flight”) system, and help activate our PSNS (“rest and digest”) system. Just like every other skill, breathing well takes practice, and practice makes perfect. Specifically, you may find your mind wandering and it is hard to maintain attention on your breath. That is normal, and it is okay. The more you practice, the easier it will become! These are just some basic exercises. If you need more help, a quick google or YouTube search will give you plenty of results for guided breathing exercises, which might be a good place to start if you are finding it difficult. Apps on our phones… and even smart watches, may give us reminders to breathe! They may seem like annoying notifications, especially since they probably pop up at times when we feel busy and stressed and don’t have time… but it might be worth starting to take more notice of these notifications. 2020 has shown some unprecedented times due to the COVID-19 epidemic. Many of us are under increased stress due to work or personal circumstances, or feel negative emotions such as loneliness or frustration. Why not try “breathing away” some of these negative emotions, and taking control of your health! By Angus Nicol |
HMC TEAMIf you find something of interest that might suit this space, or would like information on a specific topic, let us know at hmcosteo@gmail.com
Archives
December 2023
Categories |


 RSS Feed
RSS Feed
